Abstract
Improvements in neonatal intensive care have resulted in more extremely low birthweight babies surviving who are at risk of developing chronic lung disease. The preterm lung is vulnerable as it is both structurally immature and deficient in surfactant and antioxidant defences. Mechanical ventilation and high inspired oxygen concentrations are often necessary for preterm babies to survive but they can cause pulmonary inflammation which leads to lung damage. Abnormal healing in the presence of ongoing inflammation leads to airways remodelling which can result in protracted respiratory problems in these babies. A commonly used definition for chronic lung disease is the requirement for supplemental oxygen beyond 36 weeks’ postconception.
Many drugs that are commonly used for chronic lung disease have not been subjected to proper randomised controlled trials but are widely used on the basis of small studies showing short term benefits. They can be broadly divided into 2 groups. First, there are preventative drugs that are administered early to reduce oxygen toxicity and pulmonary inflammation. Secondly, there are those administered in established chronic lung disease, designed to reduce respiratory morbidity. Pulmonary inflammation in the neonate is reduced by systemic corticosteroids. Corticosteroid therapy within the first 2 weeks of life enables earlier extubation of preterm babies with subsequent reduced chronic lung disease and improved neonatal survival when given between 7 and 14 days. However, there is an increased risk of gastrointestinal haemorrhage, metabolic derangement, ventricular hypertrophy and potential effects on long term growth and brain development. Diuretics and inhaled bronchodilators improve pulmonary compliance and reduce oxygen requirements in established chronic lung disease but probably have little effect in reducing the incidence. In babies with established chronic lung disease, home oxygen therapy enables earlier discharge and prophylaxis against respiratory syncytial virus can reduce morbidity from bronchiolitis. All of the above therapies have adverse effects that need to be considered before initiating treatment.
Recently, new drugs have become available which may be beneficial. These include inhaled nitric oxide for reduction of ventilation-perfusion mismatching, recombinant human superoxide dismutase for protection against oxidative stress and alpha-1 proteinase inhibitor which may reduce airways remodelling. At present these therapies are undergoing clinical trials. Exogenous surfactant is beneficial in respiratory distress syndrome and may reduce the risk of chronic lung disease but there have been no randomised controlled trials of its use in established chronic lung disease. Drugs which have been tried unsuccessfully include erythromycin, ambroxol and mast cell stabilisers.
Similar content being viewed by others
1. Pathogenesis and Clinical Course of Neonatal Chronic Lung Disease
Neonatal chronic lung disease is a major consequence of premature delivery and prolonged neonatal intensive care. The original description in 1967 was of babies of about 34 weeks’ gestation who had required mechanical ventilation, developed a persistent oxygen requirement beyond 28 days and had the typical chest x-ray appearances of overinflation with cyst formation.[1] Advances in neonatal medicine over the past 3 decades have meant that fewer of these more mature preterm babies require mechanical ventilation and there has been a reduction in chronic lung disease in this group.[2] There are, however, many more extremely preterm, extremely low birthweight survivors and as a result, the total number of babies with chronic lung disease is increasing.[2,3] The changing preterm population has necessitated a change in the sdefinition of chronic lung disease from oxygen requirement beyond 28 days[1] to oxygen requirement beyond 36 or 40 weeks’ postconception often associated with hazy opacification on chest x-ray rather than cysts and overinflation, the latter definition being more predictive of long term outcome.[4]
Chronic lung disease results from abnormal tissue repair following an acute injury to the premature lung which leads to fibrotic tissue replacing normal alveoli.[5] The preterm lung is particularly vulnerable to injury, as it is structurally immature and deficient in both surfactant and antioxidant defence mechanisms.[6,7] The initial damage probably results from ventilatory barotrauma or volutrauma disrupting the lung tissue[8] along with oxygen free radicals causing lipid membrane and DNA damage to the cells lining the airways.[7] This damaged tissue triggers an inflammatory response with inflammatory cells[9] and proinflammatory cytokines found in high levels in lung lavage fluid from babies who subsequently develop chronic lung disease.[10,11] The inflammatory process itself may be harmful, further contributing to the lung damage by increasing oxidative stress via the neutrophil respiratory burst[12] and by the release of proteolytic enzymes such as collagenases and elastase which damage the extracellular matrix of the lung.[13,14] Some babies without initial respiratory distress who do not require oxygen or ventilation may also develop pulmonary inflammation, for example as a result of maternal chorioamnionitis[15] or infection with Ureaplasma urealyticum leading to chronic lung disease.[16] Ongoing inflammation and a damaged extracellular matrix probably lead to repair by fibrosis rather than regeneration of normal lung tissue.
Lung fibrosis in chronic lung disease leads to impaired gas exchange, decreased lung compliance, airways obstruction, ventilation-perfusion mismatching and increased energy expenditure for breathing.[17,18] The airways are hyper-reactive with a tendency for bronchospasm.[19] There is associated pulmonary hypertension[20] and pulmonary oedema[21] which can rapidly worsen during acute cyanotic spells.
The incidence of chronic lung disease varies between centres but generally occurs in about 20 to 30% of newborns who require mechanical ventilation.[22,23] The incidence increases with decreasing gestation with about 85% of babies <700g being affected falling to 5% at 1500g and above.[3] Clinically, babies with chronic lung disease often have a protracted need for mechanical ventilation and supplemental oxygen. They are usually tachypnoeic with wheezing, intermittently interrupted by spells of apnoea or acute cyanosis. They remain as inpatients for longer than babies without chronic lung disease necessitating extra expense and inconvenience for their parents. They may continue to wheeze long after hospital discharge[24] and have diminished pulmonary reserve to cope with minor upper respiratory tract infections even when they no longer require supplemental oxygen.
Viral illnesses such as bronchiolitis caused by respiratory syncytial virus (RSV) frequently necessitate repeat hospital admissions and occasionally the need for repeat mechanical ventilation.[25] Increased energy expenditure for breathing coupled with poor nutrition often lead to poor growth in infancy.[26] Chronic pulmonary hypertension can lead to cor pulmonale with recurrent bouts of acute pulmonary oedema and increased risk of sudden death.[27] Developmentally, children with severe chronic lung disease do not perform as well as their peers perhaps as a result of chronic illness and early prolonged hospitalisation.[28] Eventually, with time, the majority will achieve almost normal lung function.[17]
By definition, babies with chronic lung disease will require supplemental oxygen to maintain normal arterial oxygen saturation although various drugs can influence the duration and concentration of oxygen required. A high inspired oxygen concentration can potentiate pulmonary inflammation and it is logical to endeavour to lower inspired oxygen if possible. If, however, only a low concentration of supplemental oxygen is required this is probably relatively safe and the risk-benefit ratio of the drugs used to improve lung function compared with continued oxygen therapy must be considered.
Drugs for chronic lung disease can be divided broadly into those administered early with the aim of reducing ventilation requirements and minimising oxygen toxicity, and those administered later to facilitate earlier discharge and reduce respiratory morbidity. Drugs widely used in hospital include corticosteroids, diuretics and inhaled bronchodilators and corticosteroids. After discharge, therapies include home oxygen and RSV prophylaxis with hyperimmune globulin or monoclonal antibody. Recently some innovative new therapies have been developed that are undergoing clinical trials. The aim of this review is to balance the benefits of drugs for prevention and treatment of chronic lung disease with their possible risks.
2. Corticosteroids
Inflammation plays a key role in the development of chronic lung disease[10,11] and corticosteroids can reduce inflammation in the neonatal lung.[29] Infants with respiratory distress syndrome have higher levels of endogenous cortisol than healthy neonates, presumably on the basis of a stress response[30] but levels are no different between those who subsequently develop chronic lung disease and those who do not.[31] In 1 study babies who developed chronic lung disease had low cortisol levels following adrenocorticotropic hormone stimulation during the first week of life.[32] Whether adrenal insufficiency is associated with increased risk of developing chronic lung disease is still debated.
There have been many randomised controlled trials examining benefits and risks of systemic corticosteroids for babies with or at risk of chronic lung disease.[33,34] Meta-analysis of all of the trials up to July 1999 enables the results to be studied collectively. The studies have been divided into 3 groups depending on the time of treatment after birth: (i) early treatment (<96 hours);[35] (ii) moderately early treatment (7 to 14 days);[36] and (iii) late treatment (>3 weeks).[37] In most trials dexamethasone was compared with placebo. Dexamethasone was usually given in a reducing dosage (0.5 mg/kg/day for 3 days, then 0.25 mg/kg/day for 3 days, followed by 0.12 mg/kg/day for 3 days, and finally 0.05 mg/kg/day for 3 days) although hydrocortisone has also been used[38] and other dosage regimens employed.
2.1 Benefits of Corticosteroids
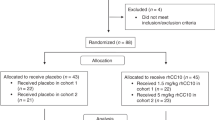
Meta-analyses of the trials of corticosteroid therapy have been summarised in the Cochrane Library (July 1999). There are 11 individual studies of early (treatment started before 4 days) corticosteroid treatment and meta-analysis showed a significant reduction in chronic lung disease at 36 weeks and more rapid weaning from mechanical ventilation (table I).[35] Meta-analysis of 6 trials of moderately early (treatment started between 7 and 14 days) corticosteroid therapy showed a reduction in neonatal mortality, earlier extubation and a reduced risk of chronic lung disease at 36 weeks (table II).[36] Meta-analysis of 8 trials of late (treatment started after 3 weeks) systemic corticosteroid treatment showed a more rapid weaning from mechanical ventilation in the corticosteroid-treated group but there was no reduction in mortality[37] (table III). Calculation of the number needed to treat (NNT)[40] enables a direct comparison of benefits and risks.
Meta-analysis of early postnatal corticosteroid therapy (<96 hours after birth) trials (after Halliday,[39] with permission)
Meta-analysis of moderately early postnatal corticosteroid therapy (7 to 14 days after birth) trials (after Halliday,[39] with permission)
Meta-analysis of late postnatal corticosteroid therapy (>3 weeks after birth) trials (after Halliday,[39] with permission)
Overall it would appear that corticosteroid administration exerts short term beneficial effects on the neonatal lung with improved lung mechanics and gas exchange that facilitate earlier extubation. The additional benefits of less chronic lung disease and a reduction in the total duration of supplemental oxygen only occurs when corticosteroids are given within the first 14 days of life. With moderately early corticosteroids the benefit of a reduced mortality at 28 days has to be balanced against the risks of this treatment.
2.2 Adverse Effects of Corticosteroids
There are many reported adverse effects of dexamethasone in preterm babies (table IV).[41] Transient hyperglycaemia is common and invariably responds to insulin therapy and reduced corticosteroid dosage. Hypertension and left ventricular hypertrophy also occur during corticosteroid treatment but resolve when it is discontinued and their long term significance is uncertain.[42] Complications such as gastrointestinal haemorrhage or perforation and growth failure are more important as they could potentially have long term implications. Linear growth ceases during dexamethasone therapy, resuming when it is discontinued.[43] There are concerns that interruption of growth during this critical early period may influence later ‘programming’ of somatic growth.
Corticosteroids may also have an effect on the developing brain. In animal studies they have been shown to reduce brain growth[44] and impair motor function.[45] Early treatment with corticosteroids is also associated with a significant decline in the rate of head growth in human newborns.[46] In 1 randomised trial corticosteroid-treated neonates had an increased number of new periventricular echodensities on cranial ultrasound scan although this was not statistically significant.[47] Although no deleterious effects on development have been demonstrated with single courses of corticosteroids given before birth,[48] recent studies have shown that corticosteroid treatment soon after birth increases the risk of abnormal neurodevelopmental outcome.[49,50] These studies had incomplete follow up of eligible surviving babies but a more recent study of the long term outcome of infants given a 42 day course of dexamethasone showed similar results even though the drug was started late rather than early.[49] The duration of therapy may be important, in addition to its timing after birth.
Data from the meta-analyses enable quantification of the magnitude of risk. For example, early corticosteroids increase the chance of gastrointestinal bleeding (table I). For every 14 babies given corticosteroids in the first 4 days of life there will be 1 extra case of gastrointestinal haemorrhage and 1 extra baby without chronic lung disease at 36 weeks (table I). For moderately early corticosteroid treatment there will be an extra case of left ventricular hypertrophy for every 5 treated compared with an extra survivor at 28 days for every 16 treated, but these estimates have quite wide 95% confidence intervals (table II). Late treatment with corticosteroids is also associated with increased risk of adverse effects balanced against earlier extubation and reduced need for further dexamethasone (table III). More worrying are the data from long term follow up studies which showed an approximate 2-fold increase in the risk of cerebral palsy and abnormal neurological assessment in babies treated early with dexamethasone[49,50] or with long courses of 4 to 6 weeks.[49,51]
On balance, it may be reasonable to administer a single, short reducing course of dexamethasone to ventilated preterm babies in whom severe chronic lung disease is felt to be evolving perhaps between 7 and 14 days after birth. This will facilitate earlier extubation, reduce the likelihood of developing a protracted requirement for supplemental oxygen and improve neonatal survival. Administration of corticosteroids to unventilated oxygen-dependent infants or those with established chronic lung disease should probably be avoided. In these situations the benefit of transiently reduced oxygen requirement needs to be weighed against the risks of known and potential adverse effects.
3. Diuretics
Pulmonary oedema is a prominent feature of early chronic lung disease[52] and can be reduced by the administration of diuretics.[53] Both loop and thiazide diuretics are used to treat chronic lung disease usually in combination with a potassium-sparing diuretic such as spironolactone. Loop diuretics such as furosemide act on the ascending loop of Henlé to block chloride reabsorption, thereby promoting sodium and water excretion. However, not all of the beneficial effects are mediated by increased diuresis. Some of the improvement in lung mechanics may be due to direct effects of furosemide on the lung as demonstrated by studies using inhaled furosemide.[54]
Thiazide diuretics inhibit sodium reabsorption in the renal tubules and are less potent than furosemide at promoting diuresis. Spironolactone is a competitive inhibitor of aldosterone and promotes sodium excretion whilst retaining potassium.
3.1 Benefits of Diuretics
Despite their widespread use, the evidence for benefit from diuretics in chronic lung disease is based on only a handful of small studies. These consistently showed that there are significant improvements in pulmonary mechanics (improved compliance and decreased resistance) following both furosemide[55–58] and thiazide[59–62] diuretics and that these changes are accompanied by improved oxygenation. However, it is less clear if these effects are sustained and whether diuretics influence outcomes such as death or duration of mechanical ventilation. In 1 controlled trial, prolonged furosemide administration was shown to reduce inspired oxygen need only during treatment without reducing the total duration of supplemental oxygen.[62] Only 1 study has reported a decreased mortality in diuretic-treated babies[63] and to date there have been no large multicentre randomised controlled trials. The benefit of a reduced requirement for inspired oxygen during treatment needs to be weighed against the possible adverse effects of long term diuretic therapy.
3.2 Adverse Effects of Diuretics
There are many adverse effects of diuretic therapy in preterm babies. In the short term, furosemide may cause fluid and electrolyte imbalance leading to volume depletion, alkalosis, hyponatraemia, hypokalaemia and hypochloraemia.[64] In addition thiazide diuretics and spironolactone can cause uraemia, hyperuricaemia, hyperkalaemia and hypomagnesaemia.[64] Prolonged furosemide therapy results in chronic hypercalciuria[65] which predisposes to nephrolithiasis, renal calcification[66] and bone mineral depletion.[65] Neonates in whom furosemide has been combined with prolonged total parenteral nutrition may also develop gallstones.[67] Furosemide is also ototoxic particularly when used in high dose and combined with aminoglycoside drugs.[68]
Diuretics are probably best restricted to short courses during bouts of suspected pulmonary oedema or cor pulmonale. If they are administered over a protracted period it is probably best to use a thiazide diuretic in combination with spironolactone. Babies receiving long term diuretic therapy should have regular assessment of their electrolyte levels and bone mineral status as well as intermittent renal ultrasound scans to rule out nephrocalcinosis. Audiology screening is justified in any sick preterm baby but particularly those who have been exposed to ototoxic drugs.
4. Inhaled Bronchodilators
Drugs are administered by inhalation in order to reach the target organ, the lungs, directly and thereby minimise the risk of systemic adverse effects. Aerosol delivery of therapeutic agents is either by metered dose inhaler with spacer or by nebulisation. Studies employing radioaerosols have shown that both techniques result in poor distribution of the drugs, with less than 1% actually being deposited where it is clinically effective.[69] Despite this, many studies have reported significant changes in pulmonary mechanics following inhaled drug therapy. [70–72] This has led to the widespread use of inhaled bronchodilators and corticosteroids despite the paucity of evidence for benefit from well designed randomised controlled trials.
4.1 Benefits of Bronchodilators
Hyper-reactivity of the bronchiolar smooth muscle is present from as early as the first week of life.[70] Bronchodilating drugs such as β2-agonists (e.g. salbutamol)[71] and anticholinergics (e.g. ipratropium bromide),[72] have beneficial effects on pulmonary compliance and resistance which can lead to short term improvements in blood gases. Despite these potential benefits there has been only 1 trial of prolonged inhaled bronchodilator therapy in babies with chronic lung disease.[73] This showed that salbutamol, either given alone or in combination with beclomethasone, had no effect on survival, duration of mechanical ventilation or oxygen therapy.
4.2 Adverse Effects of Bronchodilators
Adverse effects of inhaled β2-agonists are well documented in older children with asthma but have not been studied in the preterm infant. They can cause dysrhythmias and hypokalaemia and are associated with increased mortality when used regularly for asthma.[74] In animal studies, long term β2-adrenergic stimulation increases pulmonary smooth muscle and causes right ventricular hypertrophy, both features that are prominent in chronic lung disease.[75]
These data suggest that bronchodilators may only have a limited role in the treatment of chronic lung disease and should probably be reserved for short term exacerbations when wheezing is a prominent feature.
5. Inhaled Corticosteroids
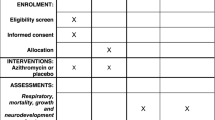
Inhaled corticosteroids are widely used for chronic lung disease without proper evidence from trials supporting tolerability or efficacy. The available studies are small and mainly published as abstracts. These have compared beclomethasone,[76] budesonide,[77] flunisolide[78] and fluticasone propionate[79] with placebo. In some studies there was a trend towards reduced time on mechanical ventilation and need for oxygen at 36 weeks in corticosteroid-treated babies but the numbers were too small to draw meaningful conclusions. The studies were summarised and subjected to a systematic review.[39] Meta-analysis showed a trend towards reduced mortality, earlier extubation and reduced chronic lung disease without a significant increase in adverse effects but the results were not statistically significant (table V). Recently, a larger study of 253 preterm babies was published as a full paper.[80] This showed no reduction in chronic lung disease in babies treated with inhaled beclomethasone but there was a reduced need for later systemic corticosteroids and less mechanical ventilation at 28 days.[80]
Meta-analysis of early postnatal inhaled corticosteroid therapy vs placebo trials (after Halliday,[39] with permission)
Inhaled and systemic corticosteroids have also been compared directly in 3 randomised trials. Although these studies were small they suggested that the effects of systemic corticosteroids on lung mechanics were more rapid than with inhaled corticosteroids. There was however, no difference in the incidence of chronic lung disease at 36 weeks between the groups.[81] A much larger trial is needed and this is currently underway to compare early (<72 hours) and late (>15 days) corticosteroid treatment, and simultaneously compare inhaled budesonide and systemic dexamethasone (the Open Study of Early Corticosteroid Treatment for the prevention of chronic lung disease in neonates with respiratory distress syndrome).[82]
6. Home Oxygen Therapy
Home oxygen therapy has been in use for over 2 decades[83] and is now becoming routinely available in most tertiary neonatal centres. Prolonged requirement of supplemental oxygen no longer necessitates inpatient care provided the caregivers can be trained in its administration from cylinders or concentrators and recognise when to seek medical assistance.
6.1 Benefits of Home Oxygen Therapy
Maintaining arterial oxygen saturation between 92 and 96% decreases pulmonary vascular resistance thereby reducing cor pulmonale.[20,27] Maintenance of adequate tissue oxygenation also improves growth[84] and reduces the incidence of apnoea and bradycardia.[85] Babies with chronic lung disease often require low concentrations of supplemental oxygen for many weeks with an increase during periods of activity such as feeding. [86] Managing babies at home enables their parents to become involved with their everyday care at an earlier stage which may improve parent-infant bonding. Savings in hospital costs have been estimated at $US40 000 per baby managed at home in 1993, although the financial burden on the family may be increased.[87]
6.2 Risks with Home Oxygen Therapy
Low dose inhaled oxygen is probably nontoxic provided it is carefully regulated. The risks with home oxygen administration are more to do with the baby being moved to an environment where the monitoring is less intense and where there is an increased risk of exposure to respiratory pathogens. It is important that families are carefully assessed for suitability before this treatment is implemented, that a reliable supply of oxygen cylinders is available and that early rapid access to a paediatrician is available if required.[88] The parents should be nonsmokers as the risk of explosion with 100% oxygen is considerable. Babies on home oxygen often require hospital re-admission during intercurrent illnesses and parents need to be taught to look for signs of increasing respiratory distress.[86] The risk of sudden infant death syndrome or acute life threatening events does not appear to be increased in babies treated with oxygen at home.[89]
7. Respiratory Syncytial Virus (RSV) Prophylaxis
Babies with chronic lung disease have poor respiratory reserve and viral infections such as bronchiolitis caused by RSV can lead to major setbacks requiring re-hospitalisation and even repeat mechanical ventilation.[90] Prophylaxis with monthly infusions of RSV immune globulin administered to babies with chronic lung disease has been shown, in randomised controlled trials, to reduce the incidence (8 vs 13.5%)[91] and severity of RSV infection.[91,92] Adverse effects from this therapy are generally mild and include fluid overload, fever and decreased oxygen saturation which occur in about 5% of treated babies.[92] Major drawbacks of this treatment are the cost and the inconvenience of regular hospital attendance for drug administration.
The recent development of a monoclonal antibody has meant that RSV prophylaxis can be administered as a series of intramuscular injections,[93] although it has been calculated that as many as 24 babies may require treatment over the winter months in order to avoid 1 single episode of re-hospitalisation.[94] Attempts to use RSV immune globulin in high risk babies with established RSV infection have not been successful.[95] Recently, a vaccine has been developed which has been shown to be both well tolerated and effective,[96] and hopefully immunisation for prevention of RSV infection will be available in the near future.
8. Benefits and Risks of Potential New Therapies for Chronic Lung Disease
Improvements in our understanding of the molecular physiology of respiratory disease and the pathogenesis of chronic lung disease have led to the development of some innovative therapies. Collectively these drugs can potentially reduce oxygen toxicity and improve pulmonary function but before they come into widespread use they need to be subjected to rigorously conducted double-blind, randomised, controlled trials.
8.1 Inhaled Nitric Oxide
Pulmonary hypertension and ventilation-perfusion mismatching are found in babies with chronic lung disease. Nitric oxide is a potent vasodilator and inhaled nitric oxide can selectively reduce pulmonary hypertension and improve oxygenation without having effects on the systemic circulation. Nitric oxide therapy clearly reduces the need for extracorporeal membrane oxygenation therapy in term infants with persistent pulmonary hypertension[97] but there are very few studies involving preterm babies. Theoretically, inhaled nitric oxide in babies with early chronic lung disease should reduce pulmonary vascular resistance and selectively increase blood flow to areas of lung that are being adequately ventilated, thereby improving oxygenation and reducing ventilation requirements and the risk of oxygen toxicity. These possible benefits would need to be weighed against the possible adverse effects of nitric oxide, including effects on platelets and bleeding,[98] possible interactions with surfactant,[99] and increased pulmonary inflammation.[100]
The available data from preterm babies with respiratory distress syndrome show that inhaled nitric oxide results in improved oxygenation, but the studies were too small to demonstrate differences in long term outcome.[101,102] In 1 study there was a worrying 64% incidence of intracranial haemorrhage.[103] Further research is obviously needed before inhaled nitric oxide can be recommended for babies at risk of chronic lung disease. At present, a multicentre collaborative trial is underway in the UK; a randomised controlled trial of ventilatory support with inhaled nitric oxide compared with ventilatory support without inhaled nitric oxide for neonates with severe respiratory failure. This trial may be able to determine if inhaled nitric oxide can prevent chronic lung disease.[82]
8.2 Antioxidant Therapy
Antioxidants such as retinol (vitamin A), tocopherol (vitamin E) and the enzyme, superoxide dismutase have been administered to preterm babies at risk of chronic lung disease in an attempt to reduce oxygen free radical-induced lung inflammation. Retinol[104] and tocopherol[105] have not been shown to improve outcome in randomised trials but superoxide dismutase has shown some promise. Endogenous pulmonary superoxide dismutase levels increase with increasing length of gestation in fetal postmortem specimens.[106] Superoxide dismutase in combination with other antioxidants probably provides the first line of antioxidant defence. Early clinical trials with subcutaneously administered superoxide dismutase from a bovine source were disappointing.[107] More recently, recombinant human superoxide dismutase has been shown in animal studies to significantly reduce the lung damage caused by hyperoxia and hyperventilation when administered intratracheally.[108] Pharmacokinetic studies in human infants have demonstrated that recombinant human superoxide dismutase can be safely administered directly into the lungs and that this results in a significant increase in the antioxidant activity of the lung lavage fluid.[109,110] At present there are no studies large enough to demonstrate significant differences in clinical outcomes in infants who have received this therapy, but these are currently being undertaken in the US.
Selenium is an essential component of another important antioxidant, the enzyme glutathione peroxidase. Preterm babies become selenium depleted[111] and low levels of selenium are associated with increased respiratory morbidity.[112] Selenium repletion protects neonatal rat lungs from the effects of hyperoxia,[113] and preliminary human studies suggest that selenium supplementation to human newborns is well tolerated.[114] To date, there are no published randomised controlled trials large enough to show whether or not selenium supplementation is efficacious in reducing chronic lung disease.
8.3 Alpha-1 Proteinase Inhibitor
A recent approach to preventing chronic lung disease has been to attempt to reduce the destructive effects of elastase on the lung by administering alpha-1 proteinase inhibitor (alpha-1 antitrypsin). Alpha-1 proteinase inhibitor forms a complex with neutrophil elastase thereby preventing destruction of the extracellular matrix. Intravenous alpha-1 proteinase inhibitor (60 mg/kg bodyweight) or placebo was infused on 4 occasions during the first 2 weeks of life.[115] There was a reduced relative risk [RR 0.48; confidence interval (CI) 0.23 to 1.00] of chronic lung disease at 36 weeks in the treated group which just failed to reach statistical significance, but there was a significant reduction in the incidence of pulmonary haemorrhage (RR 0.22; CI 0.05 to 0.98). The treatment was well tolerated by the infants and further studies are warranted.
8.4 Exogenous Surfactant
It is now well established that exogenous surfactant therapy is beneficial for the prevention and treatment of respiratory distress syndrome and timely surfactant therapy will probably also prevent chronic lung disease in some cases.[116] What is not clear is whether surfactant therapy would be beneficial to babies with established chronic lung disease. Although not primarily deficient in surfactant, babies with chronic lung disease may have surfactant inactivation due to leakage of serum proteins into the alveolar spaces. It has been hypothesised that surfactant supplementation in these babies may be beneficial in reducing ventilation and oxygen requirements.
Surfactant has been administered to 10 infants with early chronic lung disease who remained ventilated in more than 40% oxygen. They showed improved oxygenation over the 72 hours following treatment but long term benefits were not observed.[117] Surfactant may prove to be a useful adjunctive therapy for babies with chronic lung disease but cannot be recommended until it has been subjected to a much larger randomised controlled trial.
8.5 Antibacterials (Erythromycin)
An association between mycoplasma colonisation of the lower airways and the development of chronic lung disease has led to speculation that organisms such as Ureaplasma urealyticum may contribute to the prolonged pulmonary inflammatory response seen in these infants.[16,118] One study suggested that if babies were culture positive they had more than a 10-fold greater risk of chronic lung disease [119] In a randomised, double-blind, placebo-controlled trial of erythromycin therapy (15 mg/kg/dose 3 times daily for 1 week) in babies less than 30 weeks’ gestation, the treatment group was found to have no reduction in pulmonary inflammation and no reduction in chronic lung disease.[120] Only 9 out of 75 babies were culture positive in this study but it is interesting to note that pulmonary inflammation was no greater in this group. The authors felt that the overall contribution from infection to the development of chronic lung disease was probably low and that even confining erythromycin therapy to colonised babies would probably not make a significant difference. Others have shown that ureaplasma infection is associated with a reduction of respiratory distress syndrome but an increase in chronic lung disease independent of gestational age.[118] These authors believed that treatment of affected infants after birth would be unlikely to improve outcome and that identification and treatment of women with ureaplasma infection before preterm birth was necessary.
8.6 Ambroxol
Ambroxol, a metabolite of bromhexine, may have beneficial effects on surfactant synthesis and secretion.[121] In 1 randomised controlled study of preterm babies with respiratory distress syndrome, ambroxol therapy (30 mg/kg bodyweight daily by intravenous infusion for 5 days) was shown to improve respiratory outcome at 28 days with a reduced incidence of chronic lung disease (29 vs 54%) and lower oxygen requirements.[122] The methodology of this study has been criticised because 31 of the 179 babies enrolled were not included in the final analysis. The same authors have recently shown only a very modest improvement in lung compliance over 4 weeks following ambroxol treatment[123] and this therapy is unlikely to become part of the routine management of babies at risk of chronic lung disease.[116]
8.7 Mast Cell Stabilisers
Both systemic (ketotifen) and inhaled (sodium cromoglycate) mast cell stabilisers have been used in an attempt to reduce the incidence and severity of chronic lung disease. A randomised controlled trial of ketotifen therapy reported fewer symptoms and reduced need for other medications in the treatment group.[124] However, the value of this study was limited by the fact that it was not blinded and no differences in objective outcomes were demonstrated. A blinded randomised study of aerosolised sodium cromoglycate failed to show any reduction in bronchopulmonary dysplasia in the treatment group.[125] At present, it seems there are no indications for mast cell stabilisers in preterm babies.
8.8 Antileukotrienes
Leukotrienes are products of arachidonic acid metabolism and have been shown to be involved in airways inflammation in asthma. Antileukotriene drugs have been demonstrated to reduce bronchoconstriction and improve symptomatology in asthma.[126] The role of leukotrienes in chronic lung disease has not been studied. If leukotrienes are involved in this disease then antileukotriene drugs may offer new therapeutic opportunities.
9. Conclusions
Chronic lung disease remains a major problem facing neonatologists and paediatricians. Many of the drugs that are used to treat chronic lung disease have not been subjected to proper randomised controlled trials. Although the efficacy of some drugs is unproven they are almost certainly beneficial in certain circumstances, and it is likely that they will continue to be used in the absence of a viable alternative. It is therefore essential that there are clear therapeutic objectives before prescribing them and that the potential adverse effects of the drugs are considered in the context of these objectives. For example, if it is believed that a reduction in the time spent on mechanical ventilation at high concentrations of inspired oxygen is the key to reducing chronic lung disease, it might be reasonable to use powerful drugs such as corticosteroids which have been proven to facilitate earlier extubation in spite of the risk of serious adverse effects.
Similarly, it would be reasonable to use drugs that improve pulmonary compliance, such as diuretics and bronchodilators, if these were believed to facilitate earlier extubation, or reduce the inspired oxygen concentration from toxic levels to better tolerated lower levels. It is less clear, however, if drug treatment is justified in babies with chronic lung disease who require only low to moderate concentrations of supplemental oxygen. Low dose oxygen is relatively well tolerated and although corticosteroids, diuretics and bronchodilators will reduce the requirement for oxygen, this will be at the expense of the numerous adverse effects. A safer alternative may be to manage these infants with supplemental oxygen at home and reserve drug treatment for periods of exacerbation or intercurrent illness.
Another important consideration is financial cost. Many drugs that are commonly used for chronic lung disease are inexpensive and may be used to facilitate earlier discharge to reduce the cost of inpatient care. Provision of home oxygen therapy will somewhat circumvent this argument. With RSV prophylaxis, the issue of cost has also generated great debate. Although RSV prophylaxis is proven to be well tolerated and of therapeutic benefit, the drugs are expensive and also costly in terms of the commitment required to attend for regular antibody administration. This expense and inconvenience needs to be weighed against what is a fairly modest reduction in the incidence of RSV requiring hospitalisation.
In the future it is likely that new drugs will be available that can reduce oxygen toxicity and prevent progression to pulmonary fibrosis. It must be borne in mind, however, that chronic lung disease does not have a single simple pathogenesis and new specific treatments may not be easy to develop. Recombinant human superoxide dismutase and alpha-1 proteinase inhibitor appear relatively well tolerated but their efficacy is not yet proven. The role of inhaled nitric oxide is also yet to be defined. Although there is short term improved oxygenation with inhaled nitric oxide, some of its metabolites may potentially increase respiratory inflammation. With time the benefits and adverse effects of these newer treatments will become clearer, but until then they should only be used with caution within the context of clinical trials. Unfortunately, there remain too many unproven treatments for neonatal chronic lung disease.[127]
References
Northway WH, Rosan RC, Porter DY. Pulmonary disease following respirator therapy of hyaline membrane disease: bronchopulmonary dysplasia. N Engl J Med 1967; 276: 357–68
Northway WH. Bronchopulmonary dysplasia: then and now. Arch Dis Child 1990; 65: 1071–81
Parker RA, Lindstrom DP, Cotton RB. Improved survival accounts for most but not all of the increase in bronchopulmonary dysplasia. Pediatrics 1992; 90: 663–8
Shennan AT, Dunn MS, Ohlsson A, et al. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics 1988; 82: 527–32
Bonikos DS, Bensch KG, Northway WH, et al. Bronchopulmonary dysplasia: the pulmonary pathologic sequel of necrotising bronchiolitis and pulmonary fibrosis. Hum Pathol 1976; 7: 623–50
Philip AGS. Oxygen plus pressure plus time: the etiology of bronchopulmonary dysplasia. Pediatrics 1975; 55: 44–50
Saugstad OD. Chronic lung disease: the role of oxidative stress. Biol Neonate 1998; 74Suppl. 1: 21–8
Bjorklund LJ, Ingimarsson J, Curstedt T, et al. Manual ventilation with a few large breaths at birth compromises the therapeutic effect of surfactant in immature lambs. Pediatr Res 1997; 42: 348–55
Merritt TA, Stuard ID, Puccia J, et al. Newborn tracheal aspirate cytology: classification during respiratory distress syndrome and bronchopulmonary dysplasia. J Pediatr 1981; 98: 949–56
Groneck P, Gotze-Speer B, Oppermann M, et al. Association of pulmonary inflammation and increased microvascular permeability during the development of bronchopulmonary dysplasia: a sequential analysis of inflammatory mediators in respiratory fluids of high risk preterm neonates. Pediatrics 1994; 93: 712–8
Kotecha S, Chan B, Azam N, et al. Increase in interleukin-8 and soluble intercellular adhesion molecule-1 in broncho-alveolar lavage fluid from premature infants who develop chronic lung disease. Arch Dis Child 1995; 72: F90–F6
Brus F, van Oeveren W, Okken A, et al. Activation of circulating polymorphonuclear leukocytes in preterm infants with severe idiopathic respiratory distress syndrome. Pediatr Res 1996; 39: 456–63
Sweet DG, Pizzoti J, Wilbourn M, et al. Matrix metalloproteinase-9 (MMP-9) in the airways of infants at risk of developing chronic lung disease (CLD) [abstract]. Eur Respir J 1999; 14Suppl. 30: 248s
Watterberg KL, Carmichael DF, Gerdes JS, et al. Secretory leukocyte protease inhibitor and lung inflammation in developing bronchopulmonary dysplasia. J Pediatr 1994; 125: 264–9
Watterberg KL, Demers LM, Scott SM, et al. Chorioamnionitis and early lung inflammation in infants in whom bronchopulmonary dysplasia develops. Pediatrics 1996; 97: 210–5
Cassell GH, Waites KB, Crouse DT, et al. Association of Ureaplasma urealyticum infection of the lower respiratory tract with chronic lung disease and death in very-low-birth-weight-infants. Lancet 1988; II: 240–5
Gerhardt T, Hehre D, Feller R, et al. Serial determination of pulmonary function in infants with chronic lung disease. J Pediatr 1987; 110: 448–56
De Meer K, Westerterp KR, Houwen RH, et al. Total energy expenditure in infants with bronchopulmonary dysplasia is associated with respiratory status. Eur J Pediatr 1997; 156: 299–304
Motoyama EK, Fort MD, Klesh KW, et al. Early onset of airway reactivity in premature infants with bronchopulmonary dysplasia. Am Rev Resp Dis 1987; 136: 50–7
Halliday HL, Dumpit FM, Brady JP. Effects of inspired oxygen on echocardiographic assessment of pulmonary vascular resistance and myocardial contractility in bronchopulmonary dysplasia. Pediatrics 1980; 65: 536–40
Jeffries AN, Coates G, O’Brodovich H. Pulmonary epithelial permeability in hyaline membrane disease. N Engl J Med 1984; 311: 1075–80
Avery ME, Tooley WH, Keller JB, et al. Is chronic lung disease in low birth weight infants preventable? A survey of 8 centers. Pediatrics 1987; 79: 26–30
Corcoran JD, Patterson CC, Thomas PS, et al. Reduction in the risk of bronchopulmonary dysplasia from 1980-1990: results of a multivariate logistic regression analysis. Eur J Pediatr 1993; 152: 677–81
Elder DE, Hagan R, Evans SF, et al. Recurrent wheezing in very preterm infants. Arch Dis Child 1996; 74: F165–F71
Meert K, Heidemann S, Lieh-Lai M, et al. Clinical characteristics of respiratory syncytial virus infections in healthy versus previously compromised host. Pediatr Pulmonol 1989; 7: 167–70
Chye JK, Gray PH. Rehospitalization and growth of infants with bronchopulmonary dysplasia: a matched control study. J Paediatr Child Health 1995; 31: 105–11
Abman SH, Wolfe RR, Accurso FJ, et al. Pulmonary vascular response to oxygen in infants with severe bronchopulmonary dysplasia. Pediatrics 1985; 75: 80–4
Gregoire MC, Lefebvre F, Glorieux J. Health and developmental outcomes at 18 months in very preterm infants with bronchopulmonary dysplasia. Pediatrics 1998; 101: 856–69
Groneck P, Reuss D, Goetze-Speer B, et al. Effects of dexamethasone on chemotactic activity and inflammatory mediators in tracheobronchial aspirates of preterm infants at risk for chronic lung disease. J Pediatr 1993; 122: 938–44
Baden M, Bauer C, Colle E, et al. Plasma corticosteroids in infants with the respiratory distress syndrome. Pediatrics 1973; 52: 782–7
Merz U, Pfaffle R, Peschgens T, et al. The hypothalamic-pituitary-adrenal axis in preterm infants weighing < 1251g: association with perinatal data and chronic lung disease. Acta Paediatr 1998; 87: 313–7
Watterberg KL, Scott SM. Evidence of early adrenal insufficiency in babies who develop bronchopulmonary dysplasia. Pediatrics 1995; 95: 120–5
Halliday HL. A review of postnatal corticosteroids for treatment and prevention of chronic lung disease in the preterm infant. Prenat Neonatol Med 1997; 2: 1–12
Bhuta T, Ohlsson A. Systematic review and meta-analysis of early postnatal dexamethasone for prevention of chronic lung disease. Arch Dis Child 1998; 79: F26–F33
Halliday HL, Ehrenkranz RA. Early postnatal (<96 hours) corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Library, Update Software, Oxford, Issue 3, 1999
Halliday HL, Ehrenkranz RA. Moderately early (7-14 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Library, Update Software, Oxford, Issue 3, 1999
Halliday HL, Ehrenkranz RA. Delayed (> 3 weeks) postnatal corticosteroids for chronic lung disease in preterm infants. Cochrane Library, Update Software, Oxford, Issue 3, 1999
Baden M, Bauer CR, Cole E, et al. A controlled trial of hydrocortisone therapy in infants with respiratory distress syndrome. Pediatrics 1972; 50: 526–34
Halliday HL. Clinical trials of postnatal corticosteroids: inhaled and systemic. Biol Neonate 1999; 76Suppl. 1: 29–40
Cook RJ, Sackett DL. The number needed to treat: a clinically useful measure of treatment effect. BMJ 1995; 310: 452–4
Ng PC. The effectiveness and side effects of dexamethasone in preterm infants with bronchopulmonary dysplasia. Arch Dis Child 1993; 68: F330–F6
Werner JC, Sicard RE, Hansen TRW, et al. Hypertrophic cardiomyopathy associated with dexamethasone therapy for bronchopulmonary dysplasia. J Pediatr 1992; 120: 286–91
Gibson AT, Pearse RG, Wales JK. Growth retardation after dexamethasone administration: assessment by knemometry. Arch Dis Child 1993; 69: F505–F9
Howard E, Benjamins JA. DNA, ganglioside and sulfatide in brains of rats given corticosterone in infancy, with an estimate of cell loss during development. Brain Res 1975; 92: 73–87
Gramsbergen A, Mulder EJH. The influence of betamethasone and dexamethasone on motor development in young rats. Pediatr Res 1998; 44: 105–10
Papile LA, Tyson JE, Stoll BJ, et al. A multicenter trial of two dexamethasone regimens in ventilator-dependent premature infants. N Engl J Med 1998; 338: 1112–8
Noble-Jameison CM, Reger R, Silverman M. Dexamethasone in neonatal chronic lung disease: pulmonary effects and intracranial complications. Eur J Pediatr 1989; 148: 365–7
Collaborative Group on Antenatal Steroid Therapy. Effects of antenatal dexamethasone administration in the infant: long term follow up. J Pediatr 1984; 104: 259–67
Yeh TF, Lin YJ, Huang CC, et al. Early dexamethasone therapy in preterm infants: a follow-up study. Pediatrics 1998; 101: e7
Shinwell ES, Karplus M, Reich D, et al. Early dexamethasone therapy is associated with increased incidence of cerebral palsey. In: Hot topics’ 99 in neonatology. Washington, 1999: 240–54
O’Shea TM, Kothadia JM, Klinepeter KL, et al. Randomized placebo-controlled trial of a 42-day tapering course of dexamethasone to reduce the duration of ventilator dependency in very low birth weight infants: outcome of study participants at 1-year adjusted age. Pediatrics 1999; 104: 15–21
Edwards DK, Colby TV, Northway WH. Radiographic pathologic correlation in bronchopulmonary dysplasia. J Pediatr 1979; 95: 834–6
Demling R, Will JA. The effect of furosemide on the pulmonary transvascular fluid filtration rate. Crit Care Med 1978; 6: 317–9
Kugelman A, Durand M, Garg M. Pulmonary effect of inhaled furosemide in ventilated infants with severe bronchopulmonary dysplasia. Pediatrics 1997; 99: 71–5
Kao LC, Warburton D, Sargent CW, et al. Furosemide acutely decreases airways resistance in chronic bronchopulmonary dysplasia. J Pediatr 1983; 103: 624–9
McCann EM, Lewis K, Deming DD, et al. Controlled trial of furosemide therapy in infants with chronic lung disease. J Pediatr 1985; 106: 957–62
Engelhardt B, Elliot S, Hazinski TA. Short- and long-term effects of furosemide on lung function in infants with bronchopulmonary dysplasia. J Pediatr 1986; 109: 1034–9
Rush MG, Engelhardt B, Parker RA, et al. Double-blind, placebo-controlled trial of alternate-day furosemide therapy in infants with chronic bronchopulmonary dysplasia. J Pediatr 1990; 117: 112–8
Kao LC, Warburton D, Cheng MH, et al. Effects of oral diuretics on pulmonary mechanics in infants with bronchopulmonary dysplasia: results of a double blind crossover sequential trial. Pediatrics 1984; 74: 37–44
Kao LC, Durand DJ, Phillips BL, et al. Oral theophylline and diuretics improve pulmonary mechanics in infants with bronchopulmonary dysplasia. J Pediatr 1987; 111: 439–44
Engelhardt B, Blalock WA, DonLevy LS, et al. Effect of spironolactone-hydrochlorthiazide on lung function in infants with bronchopulmonary dysplasia. J Pediatr 1989; 114: 619–24
Kao LC, Durand DJ, McCrea RC, et al. Randomised trial of long-term diuretic therapy for infants with oxygen dependent bronchopulmonary dysplasia. J Pediatr 1994; 124: 772–81
Albersheim SG, Solimano AJ, Sharma AK, et al. Randomized, double-blind, controlled trial of long-term diuretic therapy for bronchopulmonary dysplasia. J Pediatr 1989; 115: 615–20
Davis JM, Sinkin RA, Aranda JV. Drug therapy for bronchopulmonary dysplasia. Pediatr Pulmonol 1990; 8: 117–25
Atkinson SA, Shah JK, McGee C, et al. Mineral excretion in premature infants receiving various diuretic therapies. J Pediatr 1988; 113: 540–5
Woolfield N, Haslam R, Le Quesne G, et al. Ultrasound diagnosis of nephrocalcinosis in preterm infants. Arch Dis Child 1988; 63: 86–8
Randall LH, Shaddy RE, Sturtevant JE, et al. Cholelithiasis in infants receiving furosemide: a prospective study of the incidence and one-year follow-up. J Perinatol 1992; 12: 107–11
Borradori C, Fawer CL, Buclin T, et al. Risk factors of sensorineural hearing loss in preterm infants. Biol Neonate 1997; 71: 1–10
Fok TF, Monkman S, Dolovich M, et al. Efficiency of aerosol medication delivery from a metered dose inhaler versus jet nebulizer in infants with bronchopulmonary dysplasia. Pediatr Pulmonol 1996; 21: 301–9
Rotschild A, Solimano A, Puterman M, et al. Increased compliance in response to salbutamol in premature infants with developing bronchopulmonary dysplasia. J Pediatr 1989; 115: 984–91
Barrington KJ, Finer NN. Treatment of bronchopulmonary dysplasia. Clin Perinatol 1998; 25: 177–203
Brundage KL, Mohsini KG, Froese AB, et al. Bronchodilator response to ipratropium bromide in infants with bronchopulmonary dysplasia. Am Rev Resp Dis 1990; 142: 1137–42
Denjean A, Paris-Llado J, Zupan V, et al. Inhaled salbutamol and beclomethasone for preventing broncho-pulmonary dysplasia: a randomised double-blind study. Eur J Pediatr 1998; 157: 926–31
Barrett TE, Strom BL. Inhaled beta-adrenergic receptor agonists in asthma: more harm than good? Am J Resp Dis Crit Care Med 1995; 151: 574–7
Winter R, Collins C, Ruddock PE, et al. The effect of systemic beta-2 adrenergic receptor agonist therapy on the pulmonary hypertensive response to chronic hypoxia in rats. Am Rev Resp Dis 1986; 134: 753–7
Giep T, Raibble P, Zuerlin T, et al. Trial of beclomethasone dipropionate by metered dose inhaler in ventilator dependent neonates less than 1500g. Am J Perinatol 1996; 13: 5–9
Merz U, Kusenbach G, Hausler M, et al. Inhaled budesonide in ventilator-dependent preterm infants: a randomised, double blind pilot study. Biol Neonate 1999; 75: 46–53
Townsend SF, Hale KA, Thilo EH. Early treatment with inhaled steroids does not improve outcome in extremely premature infants with respiratory distress [abstract 1763]. Pediatr Res 1998; 43: 300A
Fok TF, Lam K, Dolovich M, et al. Early use of inhaled corticosteroid in preterm infants with respiratory distress syndrome: a randomised controlled study. Arch Dis Child 1999; 80: F203–F8
Cole CH, Colton T, Shah BL, et al. Early inhaled glucocorticoid therapy to prevent bronchopulmonary dysplasia. N Engl J Med 1999; 340: 1005–10
Dimitriou G, Greenough A, Giffin FJ, et al. Inhaled versus systemic steroids in chronic oxygen dependency of preterm infants. Eur J Pediatr 1997; 156: 51–5
OSECT and INNOVO abstract available from the British Association of Perinatal Medicine Perinatal Clinical Trials Group Newsletter 1998; 13 (Winter)
Pinney MA, Cotton EK. Home management of bronchopulmonary dysplasia. Pediatrics 1978; 61: 856–9
Groothuis JR, Rosenberg AA. Home oxygen promotes weight gain in infants with bronchopulmonary dysplasia. Am J Dis Child 1987; 141: 992–5
Garg M, Kurzner SI, Batista D, et al. Hypoxic arousal responses in infants with bronchopulmonary dysplasia. Pediatrics 1988; 82: 59–63
Hudak BB, Allen MC, Hudak ML, et al. Home oxygen therapy for chronic lung disease in extremely low birth weight infants. Am J Dis Child 1989; 143: 357–60
McAleese KA, Knapp MA, Rhodes TT. Financial and emotional cost of bronchopulmonary dysplasia. Clin Pediatr 1993; 32: 393–400
Greenough A, Hird MF, Gamsu HR. Home oxygen therapy following neonatal intensive care. Early Hum Dev 1991; 26: 29–35
Gray PH, Rogers Y. Are infants with bronchopulmonary dysplasia at risk for sudden infant death syndrome? Pediatrics 1994; 93: 774–7
Cunningham CK, McMillan JA. Rehospitalisation for respiratory illness in infants of less than 32 weeks’ gestation. Pediatrics 1991; 88: 527–32
The PREVENT Study Group. Reduction of respiratory syncitial virus hospitalization among premature infants with bronchopulmonary dysplasia using respiratory syncytial virus immune globulin prophylaxis. Pediatrics 1997; 99: 93–9
Groothuis JR, Simoes EA, Levin MJ, et al. Prophylactic administration of respiratory syncytial virus immune globulin to high-risk infants and young children. The Respiratory Syncitial Virus Immune Globulin Study Group. N Engl J Med 1993; 18: 1524–30
American Academy of Pediatrics Committee on Infectious Diseases and Committee of Fetus and Newborn. Prevention of respiratory syncytial virus infections: indications for the use of palivizumab and update on the use of RSV-IVIV. Pediatrics 1998; 102: 1211–6
Robbins JM, Tilford JM, Jacobs RF, et al. A number needed to treat analysis of the use of respiratory syncytial virus immune globulin to prevent hospitalisation. Arch Pediatr Adolesc Med 1998; 152: 358–66
Rodriguez WJ, Gruber WC, Welliver RC, et al. Respiratory syncytial virus (RSV) immune globulin intravenous therapy for RSV lower respiratory tract infection in infants and young children at high risk of severe RSV infections: Respiratory Syncytial Virus Immune Globulin Study Group. Pediatrics 1997; 99: 454–61
Groothuis JR, King SJ, Hogerman DA, et al. Safety and immunogenicity of a purified F protein respiratory syncytial virus (PEP-2) vaccine in seropositive children with bronchopulmonary dysplasia. J Infect Dis 1998; 177: 467–9
Finer NN, Barrington KJ. Nitric oxide in respiratory failure in the newborn infant. Semin Perinatol 1997; 21: 426–40
Hogman M, Frostell C, Arnberg H, et al. Bleeding time prolongation and NO inhalation. Lancet 1993; 341: 1664–5
Hallman M, Waffarn F, Bry K, et al. Surfactant dysfunction after inhalation of nitric oxide. J Appl Physiol 1996; 80: 2026–34
Robbins CG, Davis JM, Merritt TA, et al. Combined effects of nitric oxide and hyperoxia on surfactant function and pulmonary inflammation. Am J Physiol 1995; 269: L545–L50
Subhedar NV, Ryan SW, Shaw NJ. Open randomised controlled trial of inhaled nitric oxide and early dexamethasone in high-risk preterm infants. Arch Dis Child 1997; 77: F185–F90
Subhedar NV, Shaw NJ. Changes in oxygenation and pulmonary haemodynamics in preterm infants treated with inhaled nitric oxide. Arch Dis Child 1997; 77: F191–F7
Meurs KP, Rhine WD, Asselin JM, et al. Response of premature infants with severe respiratory failure to inhaled nitric oxide. Preemie NO Collaborative Group. Pediatr Pulmonol 1997; 24: 319–23
Pearson E, Bose C, Snidow T, et al. Trial ofvitamin A supplementation in very low birth weight infants at risk for bronchopulmonary dysplasia. J Pediatr 1992; 121: 420–7
Watts JL, Milner R, Zipursky A, et al. Failure of supplementation with vitamin E to prevent bronchopulmonary dysplasia in infants less than 1500 g birth weight. Eur Resp J 1991; 4: 803–6
Autor AP, Frank L, Roberts RJ. Developmental characteristics of pulmonary superoxide dismutase: Relationship to idiopathic respiratory distress syndrome. Pediatr Res 1976; 10: 154–8
Rosenfeld W, Evans H, Concepcion L, et al. Prevention of bronchopulmonary dysplasia by administration of bovine superoxide dismutase in preterm infants with respiratory distress syndrome. J Pediatr 1984; 105: 781–5
Davis JM, Rosenfeld WN, Sanders RJ, et al. Prophylactic effects of recombinant human superoxide dismutase in neonatal lung injury. J Appl Physiol 1993; 74: 2234–41
Rosenfeld WN, Davis JM, Parton L, et al. Safety and pharmacokinetics of recombinant human superoxide dismutase administered intratracheally to premature neonates with respiratory distress syndrome. Pediatrics 1996; 97: 811–7
Davis JM, Rosenfeld WN, Richter SE, et al. Safety and pharmacokinetics of multiple doses of recombinant human CuZn superoxide dismutase administered intratracheally to premature neonates with respiratory distress syndrome. Pediatrics 1997; 100: 24–30
Tubman TRJ, Halliday HL, McMaster D. Glutathione peroxidase and selenium levels in the preterm infant. Biol Neonate 1990; 58: 305–10
Barlow BA, Inder TA, Graham PJ, et al. The relationship of selenium status to respiratory outcome in the very low birth weight infant. Pediatrics 1995; 96; 314–9
Kim HY, Picciano MF, Wallig MA. Postnatal selenium repletion protects lungs of neonatal rats from hyperoxia. J Nutr 1992; 122: 1760–7
Daniels L, Gibson R, Simmer K. Randomised clinical trial of parenteral selenium supplementation in preterm infants. Arch Dis Child Fetal Neonatal Educ 1996; 74: F158–64
Stiskal JA, Dunn MS, Shennan AT, et al. Alpha-1proteinase inhibitor therapy for the prevention of chronic lung disease of prematurity: a randomized, controlled trial. Pediatrics 1998; 101: 89–94
Sweet DG, Halliday HL. Current perspectives on the drug treatment of neonatal respiratory distress syndrome. Pediatr Drugs 1999; 1: 19–30
Pandit PB, Dunn MS, Kelly EN, et al. Surfactant replacement in neonates with early chronic lung disease. Pediatrics 1995; 95: 851–4
Hannaford K, Todd DA, Jeffery H, et al. Role of Ureaplasma urealyticum in lung disease of prematurity. Arch Dis Child 1999; 81: F162–F7
Pacifico L, Panero A, Roggini M, et al. Ureaplasma urealyticum and pulmonary outcome in a neonatal intensive care population. Pediatr Infect Dis J 1997; 16: 579–86
Lyon AJ, McColm J, Middlemist L, et al. Randomised trial of erythromycin on the development of chronic lung disease in preterm infants. Arch Dis Child 1998; 78: F10–F4
Wauer RR, Smalisch G, Hammer H, et al. Ambroxol for prevention and treatment of hyaline membrane disease. Eur Resp J 1989; 2Suppl. 3: S57–S65
Wauer RR, Schmalisch G, Bohme B, et al. Randomized double-blind trial of ambroxol for the treatment of respiratory distress syndrome. Eur J Pediatr 1992; 151: 357–63
Schmalisch G, Wauer RR, Bohme B. Changes in pulmonary function in preterm infants recovering from RDS following early treatment with ambroxol: results of a randomised trial. Pediatr Pulmonol 1999; 27: 104–12
Rubaltelli FF, Dani C, Meneguzzo CZ. Ketotifen in the management of infants with bronchopulmonary dysplasia. Biol Neonate 1994; 66: 45–9
Watterberg KL, Murphy S. Failure of cromolyn sodium to reduce the incidence of bronchopulmonary dysplasia: a pilot study. The Neonatal Cromolyn Study Group. Pediatrics 1993; 91: 803–6
Smith LJ. A risk-benefit assessment of antileukotrienes in asthma. Drug Saf 1998; 19: 205–18
Jobe AH. Too many unvalidated new therapies to prevent chronic lung disease in preterm infants. J Pediatr 1998; 132: 200–2
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sweet, D.G., Halliday, H.L. A Risk-Benefit Assessment of Drugs Used for Neonatal Chronic Lung Disease. Drug-Safety 22, 389–404 (2000). https://doi.org/10.2165/00002018-200022050-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200022050-00006