Abstract
Aims To ascertain how closely in 1995, neonatologists and ophthalmologists were adhering to the national guidelines for the screening of retinopathy of prematurity (ROP, 1990) and those for screening and treatment (1995).
Methods Questionnaires about the local arrangements for the screening and treatment of retinopathy of prematurity were sent to the entire consultant membership (n = 648) of the Royal College of Ophthalmologists (RCOphth) and to the clinical directors (n= 259) of neonatal units in the UK in 1995.
Results One hundered and eighty-three ophthalmologists in the UK were identified as undertaking ROP screening and/or treatment, and ROP screening took place in 207 neonatal units. Seventy-seven per cent of the ophthalmologists either complied with or exceeded recommendations for determining which babies required screening, while 7% used criteria that would have resulted in substantially fewer babies being screened. Only 17% units and 12% ophthalmologists provided written information for parents, although 66% ophthalmologists talked to the parents of babies they screened. There was a lack of clarity about responsibilities for ensuring the continuation of screening on transfer to another hospital or on discharge to home. There was a wide range of views on the ophthalmic criteria that determined when screening examinations could cease and on the indications for treatment.
Conclusions While ROP screening is almost universally adopted in the UK, there is a need for the process to be more efficient and effective. Despite the delay in reporting this survey several issues remain extant and future guidelines should clarify and refine the criteria for screening and treatment. There is a need for improved communication with parents, and particularly for written information.
Similar content being viewed by others
Introduction
National guidelines for the screening of retinopathy of prematurity (ROP) were first drawn up in the UK in 1990 in response to preliminary results of the US-based Multicenter Trial of Cryotherapy for ROP.1 This study had demonstrated for the first time the efficacy of treatment for severe disease with the consequence that screening for ROP became a priority. To ensure an efficient and effective screening programme, specific guidance was needed about: which babies were at risk of ROP, when screening should commence, the timing and frequency of examinations, the examination technique and the criteria for treatment. These issues were covered in the 1990 guidelines produced by a working party representing the British Association of Perinatal Medicine and the then College of Ophthalmologists.2 When the guidelines were revised in 1995,3 they were extended to cover the practicalities of treatment, parental information and counselling, and the management of end-stage retinopathy.
The 5 years since the dissemination of the 1995 guidelines have seen rapid growth both in our understanding of evidence-based medicine and also in the discipline of guideline development methodology. To strengthen the evidence base for the next revision of the national guidelines, the British Association of Perinatal Medicine and the Royal College of Ophthalmologists, in collaboration with the Royal College of Paediatrics and Child Health, embarked on a 5-year research programme in 1995.
The survey findings reported here and in the accompanying paper represent the first phase of this project. Although clinical practice will have changed since 1995, the results presented in these two papers (on: (1) organisation of services; and (2) audit of national guidelines for screening and treatment) are important as they establish a historical baseline for measuring any changes in practice emerging from the most recent phase of the research, a UK case-wise audit of the screening and treatment of a cohort of babies developing stage 3 ROP in 1998. Furthermore, we have only analysed and presented those data that we consider to be still pertinent in 2002.
In this paper we report the results of a questionnaire survey of clinical directors of neonatal units and consultant ophthalmologists to ascertain how closely they were adhering to national guidelines for the screening of ROP first produced in 1990 and revised in 1995 to include ROP treatment.
Methodology
The survey methodology is described in detail in the accompanying paper. In brief, questionnaires about the local arrangements for the screening and treatment of ROP were sent to the entire consultant membership (648) of the Royal College of Ophthalmologists (RCOphth) and to the clinical directors (259) of neonatal units in the UK in 1995. The questionnaire circulation was later extended on the basis of information supplied on the neonatal unit questionnaire to include both non-consultant ophthalmologists screening for ROP and non-neonatal units caring for babies at risk of ROP. The questionnaire did not implicitly define the guidelines.
Results
Replies were received from 90% (583) of ophthalmologists and 88% of neonatologists (216); 183 ophthalmologists identified themselves as screening and/or treating babies for ROP and in 207 neonatal units babies were regularly screened for ROP.
Arrangements for the screening and treatment of ROP were analysed in terms of their compliance with the recommendations made in the 1990 and 1995 guidelines.
(1) Criteria for identifying babies at risk of ROP
-
1990 and 1995 guidelines both recommend that all babies with a birth weight of less than 1501 g and/or a gestational age of less than 32 weeks are screened. In the 1990 guideline the screening of larger babies receiving prolonged oxygen therapy was not considered necessary. This issue was not mentioned in 1995
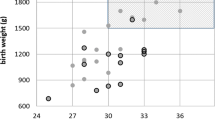
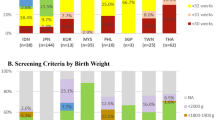
Ophthalmologists and neonatologists were asked to identify the criteria used to identify babies at risk of ROP. Excluding the 35 replies from ophthalmologists and 10 replies from neonatal units which could not be interpreted, 45% of neonatologists (88/197) and 55% (81/148) of ophthalmologists were complying with the guidelines and screening all babies less than 1501 g and/or less than 32 weeks gestation. A further 21% of units (41/197) and 22% (32/148) of ophthalmologists used criteria which would result in more babies being screened than is recommended, whereas 20% of units and 17% (25/148) of ophthalmologists used criteria which would result in slightly fewer babies being screened than if guidelines were followed strictly. However 14% of units and 7% (10/148) of ophthalmologists used criteria which suggested that substantially fewer babies were being screened than under current guidelines.
(2) Commencement of screening
-
Both 1990 and 1995 guidelines recommend the first examination should be at 6–7 weeks postnatally
One hundred and sixty ophthalmologists indicated the age at which they started ROP screening; of the 101 ophthalmologists who specified a post natal age, 75% (76) followed the guidelines by screening at 6–7 weeks; six screened first at 5–6 weeks, seven at 4 weeks, four at 3 weeks and six at 2 weeks. Fifty-five ophthalmologists provided a postmenstrual age (PMA) at which screening started; at 30 weeks (2), at 31 weeks (5); at 32 weeks (22); at 33 weeks (3); at 34 weeks (4); at 35 weeks (2); and at 36 weeks PMA (12 ophthalmologists). A further five ophthalmologists gave an age range of between 30–36 weeks PMA and four stated that they followed the RCOphth protocol.
(3) Frequency of screening examinations
-
1990 guidelines recommend that infants at risk should be examined every 2 weeks until 36 weeks postmenstrual age
-
The 1995 guidelines recommend examination every 2 weeks until vascularisation has progressed into zone 3
Of the 163 ophthalmologists who specified a frequency, 77% (126/163) followed the guidelines and screened at intervals of 1–2 weeks, 8% (13/163) screened weekly, 3% (5/163) 2–4 weekly and one, 8-weekly.
(4) Should any babies identified as at risk not be examined?
-
1990 and 1995 guidelines emphasised that the time-scale for developing serious ROP may necessitate examining the very sick neonate in an incubator, or one still receiving oxygen
The survey investigated whether screening examinations were ever postponed in a baby considered to be at risk. Ninety per cent of neonatologists (187/207) reported that there were no such circumstances when the screening would be postponed, but 10% (20) of units would postpone screening if a baby was intubated or was clinically unstable. Overall 55% (74/138) ophthalmologists stated that they never postponed screening, although 45% (64) identified specific circumstances when this might occur, such as when a baby was deemed too ill, or on the neonatologists’ advice (30%, 41), artificial ventilation (6%, 8), or baby being on oxygen (1). Four ophthalmologists gave non-medical reasons for postponement which were not being informed about the baby in time (n = 3) and parental objection (n = 1).
(5) Responsibility for ensuring follow-up screening occurs
-
1990 guideline recommendation: as infants may be transferred between neonatal units or to home before stage 3 has developed, the ophthalmologists must be able to recognise ROP with this potential and arrange for review at the appropriate time
-
1995 guideline: neonatal unit staff must inform the receiving hospital that the screening process requires to be completed, or if the infant is discharged home the appropriate follow-up appointment must be made
Ophthalmologists and clinical directors were asked who takes responsibility for ensuring follow-up screening takes place. The results presented in Table 1 show that there was a lack of clear agreement as to who takes responsibility. For babies remaining on the neonatal unit, 69% of ophthalmologists and 61% of neonatologists felt the ophthalmologist was responsible, whereas the paediatrician was felt to be responsible by 20% and 22% respectively with joint responsibility considered appropriate by 11% and 17%. However when babies were transferred to another NNU, 56% of both ophthalmologists (65/116) and 54% of neonatologists (83/148) considered that the medical staff of the receiving unit should take primary responsibility. Only 13% (15/116) of ophthalmologists and 18% (27/148) of neonatologists felt that responsibility lay with the ophthalmologist initiating screening, contrary to the 1990 guideline. When babies are discharged home the ophthalmologists are seen to take responsibility by 62% (89/143) of ophthalmologists and 59% (105/179) of neonatologists.
(6) Completion of screening examinations
-
1990 guidelines recommended screening should continue until 36 weeks PMA, or within a week, if to be discharged from hospital
-
1995 guidelines recommended screening until vascularisation has progressed into zone 3
Ophthalmologists were asked about the ophthalmic criteria used to determine when screening should cease because the risk of severe ROP had passed. One hundred and seventy-four ophthalmologists answered although 33 responses could not be interpreted. Of the replies that could be analysed, 45% (63) stated full retinal vascularisation, 23% (33) gave vascularisation into zone 3 in the absence of ROP as the criteria, and 23% (33) used partial or complete regression of ROP. Twelve ophthalmologists used a specific PMA for determining that screening should stop, in the absence of ROP, or evidence of regression, and 11 gave a PMA only; five stopped at 36 weeks, one each at 37, 38 and 39 weeks respectively, two at 40 weeks and one at 44 weeks PMA.
(7) Criteria for treatment
-
1990 and 1995 guidelines recommend the threshold for treatment to be stage 3 acute ROP involving five or more contiguous, or eight or more, cumulative clock hours in the presence of ‘plus’ disease
The 65 ophthalmologists in the survey who treated ROP were asked about their criteria for intervention (Table 2). Twenty-three of 44 ophthalmologists treating zone I ROP expressed a willingness to treat in this location before ‘threshold’ stage had been reached. Thirty-four ophthalmologists treated stage 3 ROP in zone III while 28 ophthalmologists did not state their indications for treatment.
(8) Timing of treatment
-
1990 recommendation: although the time window for treatment is around 2 weeks it is strongly recommended that treatment is undertaken within a few days of threshold diagnosis
-
1995 recommendation: treatment should be undertaken as soon as possible, ideally within 2–3 days of identification of threshold disease
When asked about the interval between the decision to treat and treatment, the replies from 65 ophthalmologists showed that 91% stated that they adhered to this recommendation and treated babies within 0–3 days although 9% delayed treatment for 4–7 days. In order to explore why treatment might be delayed ophthalmologists were asked about any circumstances which had prevented them from treating a baby at the preferred time over the previous 12 months. Although 74% of ophthalmologists reported no such circumstances, 26% (17) did do so. Of the 25 occasions when treatment was delayed, 12 were due to the clinical condition of the baby, and 13 occasions were due to non-clinical reasons; six because of no cover for annual leave, four due to problems with equipment, two because of staffing problems and once there was a difficulty with transport.
(9) Duration of follow-up after treatment
-
1990 guidelines did not cover this aspect
-
1995 guidelines recommended: all infants with stage 3 and those treated for ROP should be kept under review for at least the pre-school years
The survey showed that even before the 1995 guidelines had been disseminated this recommendation was largely being followed. Three ophthalmologists followed up children indefinitely and the mean follow-up period for the 27 specifying a precise age was 5.1 years. Five individuals followed up children until they were 3 years old, and 11 individuals continued up until 5. In all, 19 ophthalmologists continued after 5 years, and three to 16 years or beyond.
(10) Information for parents
-
1990 guideline did not cover the provision of information for parents
-
1995 guideline recommends that parents of all babies at risk of ROP should have written information about ROP as part of the general information for parents with premature babies. When severe ROP is diagnosed the ophthalmologist should personally discuss the issues with the parents with a member of neonatal unit staff present, and maintaining contact with the families of children with advanced disease is recommended
The survey asked about information given to parents; although 83% (167/202) of the neonatal units had a member of staff who routinely explained about ROP to parents of babies at risk, only 17% of units (34/205) had any printed information. Similarly only 12% of the ophthalmologists (22/184) provided printed information to supplement discussions with parents. Two thirds of ophthalmologists (66%, 112/170) saw the parents of babies they screen to provide further information and all those treating babies saw the parents of babies treated.
Discussion
The survey showed that by 1995, 7 years after the efficacy of treatment for severe ROP had been proven and 5 years after the first national UK guidelines, screening programmes for ROP had been established in almost all neonatal units within the UK. This reflects professional recognition that ROP is an important and treatable condition.
Overall the survey showed that adherence to the current UK guidelines for the screening and treatment recommendations of ROP was good. However there were some areas where apparent deviation from the recommendations could result in some babies not being screened or treated appropriately. This was most notable in relation to the identification of babies at risk of ROP, mechanisms for ensuring the screening programme is completed, and indications for intervention.
Although most units and ophthalmologists appropriately identified babies at risk of ROP in 1995, it was worrying that 14% of units and 7% ophthalmologists were using criteria which suggested that substantially fewer babies were being screened than under current guidelines. A recurring debate is whether to reduce the current upper limit for ROP screening from <1501 grams birthweight and <32 weeks GA.4,5,6,7,8,9 A UK-wide survey of stage 3 ROP that has recently been completed should help clarify this as it described the birth weight and GA characteristics of babies with severe disease and should provide evidence for future guidelines.
ROP onset and progression are mainly determined by postmenstrual rather than postnatal age,10,11 so it is illogical, as the current guidelines recommend,3 to design a screening protocol on the latter. This may be in part responsible for the diversity of the responses in this study. Perhaps future editions will titrate screening programmes according to PMA.
A clear understanding of who is responsible for ensuring follow-up screening takes place is of vital importance in maintaining a seamless programme of screening for all babies particularly those transferred between units or discharged home before screening is finished. Although there was a high degree of uniformity between clinical directors and the ophthalmologists as to who takes this responsibility, there was clearly not a unanimous view amongst either group. As the management of a comprehensive screening programme for all babies at risk depends on clear lines of communication and responsibility between neonatologists and ophthalmologists, this finding gives some cause for concern. Future guidelines should take this into account as babies being transferred to other units, or discharged to home are at particular risk of being missed from screening.12,13
ROP screening needs to be efficient and effective and to achieve this examinations need to kept to a minimum both for the sake of the baby and ophthalmologist, but to be appropriately timed so that the narrow window of opportunity for treatment is not missed. The survey found that the criteria used by many ophthalmologists for when screening should start and stop would have resulted in unnecessary examinations in some cases and too few in others. In general, there were more responses which suggested too many examinations with screening examinations commencing too early and continuing longer than necessary, often until retinal vascularisation is complete. Of more concern however, because of the implications of missing severe ROP, were the few responses that suggested screening began too late or ceased before it could be safely ascertained there was no further risk of ROP.
Currently the UK guidelines recommend treatment of ‘threshold’ ROP, defined as: stage 3 acute ROP involving five or more contiguous or eight or more cumulative clock hours in the presence of plus disease.2,3 However, contrary to the CRYO-ROP Study definition of ‘threshold’,2 the guidelines are not zone specific as described in the introduction. Overall, compliance with the guidelines in terms of indications for treatment was good. It was reassuring that compliance was highest for zone II, where most stage 3 ROP occur. The study also showed a willingness to treat zone I disease before ‘threshold’, which reflects the trend occurring in other countries and reported in the STOP-ROP Study.14 This is not surprising in view of the rarity of zone I disease (1.7% in the CRYO-ROP Study15) and poor outcome for intervention for ROP in zone I. In this respect the UK guidelines require updating.
Although nearly all the ophthalmologists treat severe ROP in zone 2, substantially fewer treated ROP in zone III. This could be because severe disease in that location is less frequent. However ROP zone may change during the acute phase due to ocular growth (zone I and II ROP have been reported to progress to zone III16) and after vascularisation of the nasal retina, the zone may be impossible to define. By convention zone is allocated as ROP first develops. In practice of course this is at the time that it is first observed; thus determining retinal zone late on in the acute phase (when the nasal retina is already vascularised) may not be possible, on the basis of one examination alone, when it is not known which zone was originally involved. ‘Threshold’ as defined by the CRYO-ROP Study, but not the UK guidelines, includes zone I and II disease only, with the implication that zone III stage 3 ROP does not require treatment. This issue needs to be taken up when the guidelines are updated, as it may be appropriate, when the zone of ROP onset is unknown, to use severity and extent alone as indications for treatment.
It was reassuring to find that once the decision to treat had been made, 91% of ophthalmologists treated within 1–3 days. Although the remaining few ophthalmologists treating after 4–7 days were still within the window of opportunity of 2 weeks specified in the 1990 guidelines, this recommendation was reduced to 2–3 days in 1995. It is of note that there were as many occasions when non-medical reasons had necessitated treatment postponement as there were occasions when the treatment had been postponed because of the clinical condition of the baby.
The area of greatest deviation from the guidelines relates to the provision of information for parents. The survey found that very few units or ophthalmologists had printed information available for parents as recommended in the revised 1995 guidelines. Whether the situation has changed in the intervening period will become evident from the cohort study referred to earlier when parents were specifically asked about the information they received and would wish to receive. This information will be used to revise the example parent information leaflets provided with the 1995 guidelines.
In conclusion, a national audit of ROP guidelines in 1995 showed that almost all neonatal units had instituted screening programmes for ROP. Recognition of which babies needed to be screened was good but there were some aspects of ROP screening and treatment which suggested both over- and under-compliance. Despite the delay in publication, this survey reports the only national survey of ROP practice with respect to screening and treatment. Here we have presented only those issues that we consider pertinent to practice in 2002, and which still need to be addressed. Thus, future guidelines should clarify and refine the criteria for initiating and discontinuing screening and the indications for treatment. There is a need for improved communication with parents, and particularly for written information.
References
Cryotherapy for Retinopathy of Prematurity Cooperative Group. Multicenter trial of cryotherapy for retinopathy of prematurity. Preliminary results. Arch Ophthalmol 1988; 106: 471–479
Anon. College News: ROP screening duty. Quart Bull Coll Ophthalmol 1990; (autumn): 6
Report of a Joint Working Party. The Royal College of Ophthalmologists, British Association of Perinatal Medicine: Retinopathy of Prematurity: guidelines for screening and treatment. Early Human Dev 1996; 46: 239–258
Fleck BW, Wright E, Dhillon B, Millar GT, Laing LA . An audit of the 1995 Royal College of Ophthalmologists guidelines for screening of retinopathy of prematurity applied retrospectively in one regional neonatal intensive care unit. Eye 1995; 9: 31–35
Goble RR, Jones HS, Fielder AR . Are we screening too many babies for retinopathy of prematurity?. Eye 1997; 11: 509–514
Pollock W, Inglesby DV, Cottrell DG . Correspondence on: An audit of the 1995 Royal College of Ophthalmologists guidelines for screening of retinopathy of prematurity applied retrospectively in one regional neonatal intensive care unit. Eye 1998; 12: 1035
Wright K, Anderson ME, Walker E, Lorch V . Should fewer premature infants be screened for retinopathy of prematurity in the managed care era?. Pediatrics 1998; 102: 31–34
Clemett R, Darlow B . Results of screening low-birth-weight infants for retinopathy of prematurity. Curr Opin Ophthalmol 1999; 10: 155–163
Joint Statement of the American Academy of Pediatrics, the American Association for Pediatric Ophthalmology and Strabismus, and the American Academy of Ophthalmology. Screening examination of premature infants for retinopathy of prematurity. Pediatrics 1997; 100: 273
Palmer EA, Flynn JT, Hardy RJ, Phelps DL et al. The Cryotherapy for Prematurity Cooperative Group. Incidence and early course of retinopathy of prematurity. Ophthalmology 1991; 98: 1628–1640
Fielder AR, Shaw DE, Robinson J, Ng YK . Natural history of retinopathy of prematurity: a prospective study. Eye 1992; 6: 233–242
Ziakas NG, Cottrell DG, Milligan DWA, Pennefather PM, Bamashmus MA, Clarke MP . Regionalisation of retinopathy of prematurity (ROP) screening improves compliance with guidelines: an audit of ROP screening in the Northern Region of England. Br J Ophthalmol 2001; 85: 807–810
Aprahamian AD, Coats DK, Paysee EA, Brady-McCreery K . Compliance with outpatient follow-up recommendations for infants at risk for retinopathy of prematurity. J AAPOS 2000; 4: 282–286
The STOP-ROP Multicenter Study Group. Supplemental therapeutic oxygen for prethreshold retinopathy of prematurity (STOP-ROP), a randomised, controlled trial 1: primary conclusions. Pediatrics 2000; 105: 295–310
Cryotherapy for Retinopathy of Prematurity Cooperative Group. The natural ocular outcome of premature birth and retinopathy. Arch Ophthalmol 1994; 112: 903–912
Repka MX, Palmer EA, Tung B for the Cryotherapy for Retinopathy of Prematurity Cooperative Group. Involution of retinopathy of prematurity. Arch Ophthalmol 2000; 118: 645–649
Acknowledgements
This study was funded by the Department of Health. We are very grateful to the Royal Colleges of Ophthalmologists and Paediatrics and Child Health for facilitating and supporting this study, and to all the ophthalmologists and clinical directors of UK neonatal units who took the time to complete the study questionnaires.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Fielder, A., Haines, L., Scrivener, R. et al. Retinopathy of prematurity in the UK II: Audit of national guidelines for screening and treatment. Eye 16, 285–291 (2002). https://doi.org/10.1038/sj.eye.6700131
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700131