Abstract
Objective:
Feeding problems are an important area of neonatal morbidity that requires attention. We defined the feeding milestones related to transition to per oral feeding among premature infants based on gestational (GA) and postmenstrual ages (PMA), and elucidated the co-morbidity variables affecting with these skills.
Study Design:
Feeding progress was tracked during the first hospitalization in a retrospective study involving 186 infants. We measured the age at acquisition of first feedings, maximum gavage feedings and maximum oral feedings. Resource usage measures included the total length of hospital stay (LOS), duration of gavage tube and duration of respiratory support. Effects of perinatal and co-morbidity factors on the acquisition of feeding milestones were evaluated. ANOVA, t-test, Wilcoxon rank sum test, χ2 test, univariate and multivariate analysis, stepwise linear regression analysis and logistic regression analysis were applied as appropriate. Data were presented as mean±s.d., or as stated. P<0.05 was considered significant.
Result:
We stratified the data into three groups based on GA at birth: <28.0 weeks (group-1), 28.0 to 32.0 weeks (group-2) and 32.0 to 35.0 weeks (group-3). Compared with group-3, group-1 needed four-fold more ventilation and five-fold more continuous positive airway pressure (CPAP) duration (all P<0.001); whereas group-2 needed two-fold more CPAP duration. Age at first feed correlated with age at full gavage feedings and age at full oral feedings (r=0.53 and r=0.71, both P<0.0001). Age at full gavage feedings correlated with age at full oral feedings (r=0.81, P<0.0001). Univariate analysis was significant for GA age, hypotension, the effects of gastroesophageal reflux, and duration of ventilation and CPAP on the PMA at maximal oral feedings (all P<0.05); multivariate analysis for these variables was also significant (R2=0.58, P<0.0001). The success rate for oral feedings at discharge accelerated with GA maturation and caffeine use; on the other hand, the need for respiratory support and management of positive blood culture were associated with failure rates (P<0.05).
Conclusion:
Infants < 28 weeks GA have significant feeding delays with respect to initiation and progression to maximal gavage and oral feedings, as well as prolonged LOS. Infants >28 weeks GA attained successful feeding milestones by similar PMA. Specific aero-digestive co-morbidities significantly affected maximal oral feeding milestone. Delays in achieving maximum gavage and maximum oral feeding milestones suggest delays with the development of control and regulation of foregut motility.
Similar content being viewed by others
Introduction
Advances in neonatal intensive care have increased survival along with the consequences of airway and digestive morbidities as well as increased resource usage to improve quality of life.1, 2, 3 Inadequate feeding capabilities in premature infants often lead to poor nutritional status and growth failure with their consequences on the subsequent stages of growth and neurodevelopmental milestones.4 Although the prevalence of feeding difficulties in premature infants is well recognized, the nature of feeding milestones including the timeline for acquisition of independent swallowing abilities as well as the impact of co-morbidity factors influencing these skills among premature neonates has not been well described. Knowledge of these facts could help with anticipatory counseling and serve as a baseline to assess feeding practice strategies within nurseries.
Swallowing is present in a fetus by 16 weeks gestation, and these functions are expected to be functional at full term birth in healthy neonates.5, 6 However, on premature birth, the evolution or acquisition of feeding skills and their timeline are not well described. Co-morbid factors, including but not limited to lung disease, patent ductus arteriosus, necrotizing enterocolitis (NEC), infections and neurological injury/impairment, can affect feeding strategies and ultimate milestones. Variability in neonatal management practices may also influence feeding strategies and outcomes.
A milestone defines the age at which a skill is achieved. Our objectives were to (1) describe feeding milestones during neonatal maturation in preterm born human neonates, and (2) identify comorbidity variables affecting acquisition of feeding milestones. In a retrospective study design from a single center academic practice physicians group operating with consensus guidelines, we tested the hypothesis that the attained feeding milestones are dependent on perinatal maturation and neonatal co-morbidities.
Methods
The Institutional Review Board of Children's Hospital of Wisconsin and the Human Research Review Committee of Medical College of Wisconsin, at Milwaukee, WI approved this study. Retrospective data from premature neonates that were admitted to the Children's Hospital of Wisconsin-NICU between January 1998 and December 1999 were evaluated. Major inclusion criterion was clear documentation of progression of feedings among infants discharged home from our institution. Exclusion criteria were (1) inadequate documentation pertinent to feeding milestones, (2) lethal anomalies and (3) syndromic infants with genetic or chromosomal disorders. Data related to feeding abilities and morbidities were collected from available subjects until discharge or death.
Nursery feeding practices related to the feeding and gastrointestinal milestones
The NICU at Children's Hospital of Wisconsin catered to both inborn and outborn neonates. The academic group of neonatologists generated and operated under consensus guidelines for the practice of standard neonatal care. The approaches to manage respiratory and feeding difficulties were similar within the group practice and were carried on by the attending neonatologist and the NICU nursing staff. Feedings were initiated when infants displayed cardiorespiratory stability. It was the unit policy that gastrointestinal tolerance was considered appropriate if pre-feeding residuals were under 50% of prior feeding volume in the presence of normal stooling pattern and with the absence of abnormal abdominal/gastrointestinal signs and symptoms (progressive abdominal distention, absence of bowel sounds, bilious aspirates). Oral feedings were initiated when infants showed oromotor cues, and feeding progress and modifications were based on cardiorespiratory stability and gastrointestinal tolerance. When feeding intolerance was present, standard evaluation and management were performed as deemed necessary. In general, there was a consensus on initiating oral feedings when infants were stable and showed oromotor cues.
In those neonates that were orally feeding well but needed supplementation for growth reasons, discharge guidelines for home gavage feeds were based on the following criteria: (1) absence of apnea and bradycardias while off xanthines, (2) enterally tolerating prescribed feeding volumes and gaining weight, (3) infants were able to be fed primarily by oral route, (4) primary caregiver has shown competency with proper gavage feeding technique, and (5) supplies and home care were available and a covered benefit was available for the patient. These practices were in accordance with existing literature on home gavage feedings.7, 8, 9
Data analysis
Data were collected related to the timing of feeding initiation, maximal feedings and the feeding methods (oral or gavage). We recorded the type and duration of respiratory support, as well as the management considerations for patent ductus arteriosus, use of steroids (antenatal or post natal) and caffeine. Demographic and morbidity characteristics, resource usage and feeding outcomes were summarized under three gestational age (GA)-based categories: (a) group-1, less than 28 weeks, (b) group-2, 28 to 32 weeks, and (c) group-3, 32 to 35 weeks at birth. This stratification is supported by the evidence that the evolution of neurodevelopmental, entero-endocrine and foregut motility markers depend on perinatal maturation.10, 11, 12, 13, 14, 15, 16, 17 Effects of co-morbidity variables and key interventions on feeding milestones (maximal gavage and maximal oral feeding) were examined with each group. Maximal feedings were considered equivalent to achieving a volume of about 120 ml kg−1 per day.18 This volume was considered maximal for the purpose of measuring a fixed milestone in all categories and to allow for fluid restriction prescribed in some conditions (patent ductus arteriosus or lung disease). Data from those subjects that truly achieved maximal gavage feeding (as defined above) are included in the evaluation of the magnitude of the co-morbidity effects (N=118); however, those subjects that advanced to oral feeding before reaching the maximal gavage milestone were not included in this analysis. Similarly, only those subjects (N=131) that truly achieved maximal oral feeding milestone are included in the evaluation of the magnitude of the co-morbidity effects.
Statistical analysis
The discrete variables were compared among the three groups with χ2 test, whereas unpaired t-tests or Wilcoxon rank sum tests analyzed the inter-group differences within the continuous outcome variables. Data were adjusted for multiple testing using the Tukey–Kramer method. Multivariate analysis was applied to examine the relationship between the confounding variables vs feeding milestones using stepwise linear regression and logistic regression for continuous and categorical variables respectively. Variables that were highly inter-correlated (r>0.80) were excluded because of multicolinearity.19, 20 Resultant data from all subjects were presented as correlation coefficients β±s.e.m. and regression values (adjusted R2) for linear regression and odds ratios with 95% confidence intervals for logistic regression. SAS (version 9.1, SAS Institute Inc., Cary, NC, USA) and MINITAB (MINITAB v15, Minitab Inc., State College, PA, USA) were used to perform the analyses. Data were presented as mean±s.d., or as stated. P<0.05 was considered significant.
Results
Demographic and morbidity characteristics
Out of 186 premature infants, data on 11 infants were excluded because of 6 deaths (4 NEC, 3 severe intraventricular hemorrhage, septic shock in all 6 deaths), 2 transfers and 3 subjects had inadequate information; thus, 175 premature infants were included. Overall, there were 54.9% males, 67.2% inborn and 48.6% born through Caesarean section. The demographic and co-morbidity characteristics are described in Table 1a and b, respectively. As anticipated, infants in group-1 (<28 weeks) had more acute morbidities, required more interventions and had more chronic morbidities compared with older premature infants. Group-2 (28 to 32 weeks) and group-3 (32 to 35 weeks) were only different in hypotension, positive blood culture and caffeine use.
Characteristics of resource usage and feeding milestones
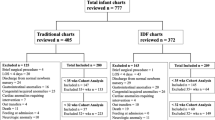
Feeding outcomes at discharge are described in Figure 1. Overall, at discharge, maximal oral feedings was achieved in 131/175 (74.9%) infants, whereas 29/175 (16.6%) were discharged on part oral and gavage feedings and 15/175 (8.6%) on gastrostomy feedings. As expected, the more premature the groups, the longer the total length of hospital stay (LOS) (Figure 2a). When looking at postmenstrual ages (PMA) at discharge, group-1 participants were discharged at 38.64±0.63 weeks PMA, group-2 at 36.73±0.48 weeks PMA and group-3 at 36.28±0.41 weeks PMA (all mean±s.e.m., group-1 vs group-2, P<0.04; and group-1 vs group-3, P<0.005).
Characteristics of feeding milestones based on PMA are described in Table 2. The PMA at 1st feeds in group-1 was 27.6±1.5 weeks, group-2 was 30.7±1.1 weeks and group-3 was 33.4±0.9 weeks (group-1 vs group-2 or group-3, P<0.05). The duration of gavage feeding (Figure 2b) included the time from 1st gavage feedings to maximal oral feedings or until discharge among those who failed to achieve independent oral feedings. Compared with group-3 infants, from the perspective of PMA, group-1 infants are more likely to start feeds earlier, achieve maximal gavage feeds at a similar PMA, but the PMA at maximal oral feeds was delayed. Group-2 infants start and reach maximal gavage feeds earlier, and are equivalent in reaching maximal oral feedings.
Correlation between initial, maximal gavage and maximal oral feedings
To test whether there was a correlation between the ages at initial feedings vs maximal gavage feedings and vs maximal oral feedings, Pearson correlation coefficients were calculated. Chronological age at first feed correlated with age at maximal gavage feedings (r=0.53) and also with age at maximal oral feedings (r=0.71) (both P<0.0001). Age at maximal gavage feedings correlated with age at maximal oral feedings (r=0.81, P<0.0001). PMA at first feed correlated with PMA at maximal gavage feedings (r=0.19, P=0.04), and also with PMA at maximal gavage feedings correlated with PMA at full oral feedings (r=0.47, P<0.0001). Thus, earlier introduction and maintenance of feeding plans may result in earlier oral feeding skills.
Relationship between co-morbidities vs maturational age at maximal gavage and oral feeding
First, using logistic regression, we tested the relationship between individual and all comorbidity factors on the ability to achieve maximal oral feeding milestone or not, and the results are shown as unadjusted and adjusted odds ratios, respectively (Table 3). Next, we tested the influence or magnitude of specific co-morbidities on the maximal gavage and maximal oral feeding milestone by using linear regression analysis, and the outputs are described in Table 4 as β±s.e.m. and adjusted R2. Univariate analysis was first performed with respect to gavage and oral feeding milestones, and significance was noted for caffeine use, presence of gastroesophageal reflux (GER), duration of ventilation and positive blood culture for gavage feeding milestone (all P<0.05); whereas, significance was noted for all the variables listed in the Table 4 for oral feeding milestones (all P<0.05). For the maximal gavage feeding milestone, significant morbidity parameters after multivariate analysis were GA, GER and duration of ventilation, whereas, for the maximal nippling milestone, significant morbidity parameters were GA, hypotension, GER, duration of ventilation and continuous positive airway pressure (CPAP).
GER subset
There were 33 (18.9%) subjects with a clinical diagnosis of GER that received treatment with acid suppressive strategy. Infants with GER had a delay in achieving maximal gavage (by 1.45 weeks, P=0.03) and maximal oral feedings (by 0.95 weeks, P=0.05) (Table 4).
Respiratory disease subset
The use of surfactant, postnatal steroids, indomethacin and surgical closure of patent ductus arteriosus were higher in <28 weeks (P<0.05, Table 1b), and the duration of ventilator and CPAP use were also higher (both, P<0.0001, Figure 3a and b). These markers of respiratory morbidities are associated with delay with attainment of feeding milestones (all P<0.05, Tables 3 and 4).
Gastrostomy subset
There were 15 neonates (7 females, 28.9±3.4 weeks GA, birth weight 1326±572 g) with G-tube as the main feeding method at discharge (N=5 in group-1, N=6 in group-2, N=4 in group-3). Major diagnoses included bronchopulmonary dysplasia (N=4), GER (N=7), severe intraventricular hemorrhage (N=2) and NEC (N=3). Fourteen of these subjects required ventilation for 28±26 days, and eight received CPAP for 16±20 days. The total LOS in this subset was 101±60 days, and nine subjects received some oral feedings at discharge.
NEC subset
Out of 175 subjects, 7 (4 females, 27.2±2.9 weeksks GA, birth weight 1049±447 g) carried the diagnosis of NEC. Co-existent morbidities included bronchopulmonary dysplasia (N=1) and severe intraventricular hemorrhage (N=3). Six were ventilated for 36±30 days and four received CPAP for 10±5 days. The total duration of hospitalization in this subset was 106±59 days. Discharge feeding methods were gastrostomy (N=3), gavage plus oral feedings (N=3) and oral feedings (N=1).
Discussion
Current clinical feeding initiation and progression practice protocols typically rely on evidences based on cardiorespiratory and gastrointestinal stability, as well as provider experience. In this retrospective study, we describe the impact of maturation and co-morbidities on the path to acquisition of the feeding milestones, an essential criterion for hospital discharge. The cardinal findings of this study are as follows: (1) infants <28 weeks GA have significant feeding delays with respect to initiation and progression to maximal gavage and oral feedings, as well as prolonged LOS; (2) infants >28 weeks GA attained successful feeding milestones by similar PMA; (3) specific aero-digestive co-morbidities significantly affected maximal oral feeding milestone; and (4) magnitude of pathophysiological characteristics impeding feeding milestones were identified.
The LOS as an indicator of economic burden of neonatal care was significantly prolonged in those born <32 weeks (vs >32 weeks). Within the former group, the feeding status among those born <28 weeks GA was different in that assisted tube feeding methods were needed in about 50% to facilitate discharge, compared with 25% of those born between 28to 32 weeks GA (Figure 1). On the contrary, only the time taken to attain maximal oral feedings was prolonged in those born >28to 32 weeks GA. Therefore, we infer that greater intrauterine maturation at birth positively affects maturation leading to independent feeding milestones at discharge. The impact of extrauterine maturation was evaluated by analyzing the PMA at which successful oral feedings were achieved. This milestone was significantly delayed in those born <28 weeks, but not among those born 28 to 32 weeks GA. These findings may be because of maturational delays in gastrointestinal motility and or because of the impact of comorbidities.7, 21, 22
Postnatal maturation in a preterm neonate can be affected by early life experiences in the form of environmental and nociceptive stimuli to the airway and digestive tract given with the intent of supporting ventilation and enteral nutrition, respectively. In this study, the duration of gavage feeding and the duration of respiratory support were significantly greater in the group born <28 weeks GA. Thus, the younger the GA, the longer these interventions are done and therefore feeding milestone delays are evident. These findings support that failed opportunities or motor restriction may delay feeding goals.23, 24, 25, 26 On the other hand, most premature infants attain maximal oral feedings by the median age of 35to 37 weeks PMA; thus, identifying maturity of this skill at this PMA as a real biologic marker may offer realistic expectations. Further studies are needed to evaluate prospective management approaches during the postnatal period to improve feeding-related quality of life in those that fall outside of these natural limits of feeding milestones.
In this study, regardless of GA, most neonates were discharged on full oral feedings before full term age (<37 weeks completed gestation). Practical implications of this finding may include that when neonates are not on the trajectory to independent oral feedings, consideration for co-morbidities as impediments to feeding success may be explored.27 Consistent with our study, many etiologies were significant impediments to the oral feeding milestone. However, relevant causes of impediments to attaining maximal gavage milestone from our study were lower GA, GER and duration of ventilation (multivariate analysis, Table 4). Similarly, impediments to achieving maximal oral feeding milestone were lower GA, hypotension, GER, duration of ventilation and CPAP (Table 4). Regardless of the impact of these co-morbidities on the PMA at the acquisition of these feeding skills, apnea of prematurity (needing caffeine), chronic lung disease (needing ventilation) and sepsis were negatively associated with oral feeding milestone (Table 3). Therefore, multidisciplinary strategies to prevent the influence of these co-morbidities are needed to affect better feeding quality of life.28The current data are in agreement with that of ours and others in that neonates with co-morbidities require additional time to show consistent oral feeding skills.18, 21, 27, 29, 30 None of these studies explored specific co-morbidity contributions to independent feeding development.
A recent study showed that introduction and achievement of independent oral feedings in healthy premature infants were attained at 34 weeks and 38 weeks, respectively.31, 32 Others contend that multiple factors are related to bottle feeding performance in preterm infants in addition to arbitrary age (GA, PMA) or weights, such as presence of oral motor skills, feeding practice and techniques.33 In our earlier study, we hypothesized that continued maturation of esophageal peristaltic reflexes, respiratory coordination during swallowing, glottal closure reflexes, and pharyngeal swallowing reflexes in healthy premature infants without co-morbidity factors may lead to independent feeding skills.34, 35, 36, 37 Typically, delays in achieving independent oral feeding stem from the concern of cardiorespiratory instability (apnea and bradycardia) or because of inappropriate esophageal and airway protection mechanisms. Recognition of the normal feeding milestones is important in the development of individualized feeding plans in the ICU neonate with co-morbidities as well. Objective evaluation of dysphagia mechanisms may result in the development of individualized feeding protocols in infants with severe feeding concerns leading to successful outcomes, shorter LOS and lower hospital costs.28 Some of this increase LOS is to be expected because of the need to allow PMA maturation that cannot necessarily be sped up. For patients outside the normal process, placement of long-term tube feeding strategies such as gastrostomy or home gavage feeds is an alternative, but is also resisted by parents. Difficulty with feeding behavior has been considered a sensitive indicator of central nervous system integrity, and may precede a diagnosis of delayed neurological development or cerebral palsy.2, 3 On the other hand, brain mechanisms of plasticity and intervention of ororhythmic-aeroingestive systems are now possible to simulate non-nutritive sucking rhythms.25, 26 Further work is needed to evaluate feeding therapies systematically.
This study offers information from a large sample related to acquisition of feeding milestones that is helpful for prognosis, feeding guidelines, estimation of LOS, parental counseling and for prospective clinical studies. Certain limitations owing to its retrospective design include (1) heterogeneity of neonatal disease or individual perinatal factors may have resulted in variability within the groups; examples may include therapeutic interventions, effect of medications or variable severity of illness. However, such variability may be minimal when physicians operate a consensus guideline; (2) within the limits of statistical strengths, we examined some confounding factors; there could be other known and unknown factors not seen in this design; (3) the characteristics of the cohort were a mix of both inborn and out born; hence variability exists in demographic and disease factors.
In summary, we characterized the impact of gestational and postnatal maturation on the attainment of maximal gavage and maximal oral feeding milestones. We further evaluated the effect of co-morbidity on feeding milestones in premature infants. Unlike measures of survival or LOS as primary outcomes, feeding milestones may be used as a yardstick for comparison of feeding related quality of life and resource usage.
Conflict of interest
The authors declare no conflict of interest.
References
Kliegman RM . Neonatal technology, perinatal survival, social consequences, and the perinatal paradox. Am J Public Health 1995; 85: 909–913.
American Academy of Pediatrics, Committee on Children with Disabilities. Managed care and children with special health care needs. Pediatrics 2004; 114: 1693–1698.
American Academy of Pediatrics, Committee on Fetus and Newborn. Hospital discharge of the high risk neonate: proposed guidelines. Pediatrics 2008; 122: 1119–1126.
Hack M, Cartar L . Growth outcomes of preterm and very low birth weight infants. In: Thureen PJ, Hay WW (eds). Neonatal Nutrition and Metabolism. 2nd edn Cambridge University Press: Cambridge, UK, 2006. pp 640–653.
Sadler TW . Special embryology: respiratory system and digestive system. In: Sadler TW (ed). Langman's Medical Embryology. 7th edn Williams and Wilkins: Baltimore, MD, 1995. pp 232–271.
Bu’Lock F, Woolridge MW, Bairn JD . Development of coordination of sucking, swallowing, and breathing: ultrasound study of term and preterm infants. Dev Med Child Neurol 1990; 32: 669–678.
AAP Guidelines. Hospital discharge of the high-risk neonate. Pediatrics 1998; 102: 411–417.
Örtenstrand A, Waldenström U, Winbladh B . Early discharge of preterm infants needing limited special care, followed by domiciliary nursing care. Acta Paediatr 1999; 88: 1024–1030.
Collins CT, Makrides M, McPhee AJ . Early discharge with home support of gavage feeding for stable preterm infants who have not established full oral feeds. Cochrane Database Syst Rev 2003; 9 (4): CD003743.
Ballard JL, Khoury JC, Wedig K, Wang L, Eilers-Walsman BL, Lipp R . New Ballard Score, expanded to include extremely premature infants. J Pediatr 1991; 119 (3): 417–423.
Dubowitz LM, Dubowitz V, Goldberg C . Clinical assessment of gestational age in the newborn infant. J Pediatr 1970; 77 (1): 1–10.
al Tawil Y, Berseth CL . Gestational and postnatal maturation of duodenal motor responses to intragastric feeding. J Pediatr 1996; 129 (3): 374–381.
Ittmann PI, Amarnath R, Berseth CL . Maturation of antroduodenal motor activity in preterm and term infants. Dig Dis Sci 1992; 37 (1): 14–19.
Berseth CL . Neonatal small intestinal motility: motor responses to feeding in term and preterm infants. J Pediatr 1990; 117 (5): 777–782.
Jadcherla SR, Klee G, Berseth CL . Regulation of migrating motor complexes by motilin and pancreatic polypeptide in human infants. Pediatr Res 1997; 42: 365–369.
Jadcherla SR, Berseth CL . Effect of erythromycin on gastroduodenal contractile activity in developing neonates. J Pediatr Gastroenterol Nutr 2002; 34: 16–22.
Jadcherla SR, Duong HQ, Hofmann C, Hoffmann RG, Shaker R . Characteristics of upper oesophageal sphincter and oesophageal body during maturation in healthy human neonates compared with adults. Neurogastroenterol Motil 2005; 17: 663–670.
Jadcherla SR, Vijayapal AS, Leuthner S . Feeding abilities in neonates with congenital heart disease: a retrospective study. J Perinatol 2009; 29 (2): 112–118.
Armitage P, Berry G . Statistical Methods in Medical Research. Blackwell Scientific Publications: Oxford, 1987.
Snedecor GW, Cochrann WG . Statistical Methods, 7th edn, The Iowa State University Press: Iowa City, IA, 1980.
Berseth CL, McCoy HH . Birth asphyxia alters neonatal intestinal motility in term neonates. Pediatrics 1992; 90 (5): 669–673.
Jadcherla SR, Berseth CL . Antroduodenal motility and feeding outcomes among neonatal extra corporeal membrane oxygenation survivors. J Pediatr Gastroenterol Nutr 2005; 41: 347–350.
Estep M, Barlow SM, Vantipalli R, Lee J, Finan D . Non-nutritive suck burst parametrics in preterm infants with RDS and oral feeding complications. J Neonatal Nurs 2008; 14 (1): 28–34.
Barlow SM, Finan DS, Chu S, Lee J . Patterns for the premature brain: synthetic orocutaneous stimulation entrains preterm infants with feeding difficulties to suck. J Perinatol 2008; 28: 541–548.
Barlow SM . Oral and respiratory control for preterm feeding. Curr Opin Otolaryngol Head Neck Surg 2009; 17: 179–186.
Poore M, Zimmerman E, Barlow SM, Wang J, Gu F . NTrainer therapy increases suck spatiotemporal stability in preterm infants. Acta Paediatr 2008; 97: 920–927.
Hawdon JM, Beauregard N, Kennedy G . Identification of Neonates at Risk of Developing Feeding Problems in Infancy. Dev Med Child Neurol 2000; 42: 235–239.
Jadcherla SR, Stoner E, Gupta A, Bates DG, Di Lorenzo C, Linscheid T . Evaluation and management of neonatal dysphagia: impact of pharyngo-esophageal motility studies and multidisciplinary feeding strategy. J Pediatr Gastroenterol Nutr 2009; 48: 186–192.
Jadcherla SR, Berseth CL . Acute and chronic intestinal motor activity responses to two infant formulas. Pediatrics 1995; 96: 331–335.
Dodrill P, Donovan T, Cleghorn G, Mcmahon S, Davie PSW . Attainment of early feeding milestones in preterm neonates. J Perinatol 2008; 28: 549–555.
Amaizu N, Shulman RJ, Schanler RJ, Lau C . Maturation of oral feeding skills in preterm infants. Acta Paediatr 2008; 97: 61–67.
Simpson C, Schanler RJ, Lau C . Early introduction of oral feeding in preterm infants. Pediatrics 2002; 110: 517–522.
Howe TH, Sheu CF, Hinojosa J, Lin J, Holzman IR . Multiple factors related to bottle-feeding performance in preterm infants. Nurs Res 2007; 56 (5): 307–311.
Jadcherla SR, Gupta A, Coley BD, Fernandez S, Shaker R . Esophago-glottal closure reflex in human infants: a novel reflex elicited with concurrent manometry and ultrasonography. Am J Gastroenterol 2007; 102: 2286–2293.
Jadcherla SR, Gupta A, Stoner E, Fernandez S, Shaker R . Pharyngeal swallowing: defining pharyngeal and upper esophageal sphincter relationships in human neonates. J Pediatr 2007; 151: 597–603.
Jadcherla SR, Duong HQ, Hoffman R, Shaker R . Esophageal body and UES motor responses due to abrupt esophageal provocation in premature infants. J Pediatr 2003; 143: 31–38.
Jadcherla SR, Hoffmann RG, Shaker R . Effect of maturation on the magnitude of mechanosensitive and chemosensitive reflexes in the premature human esophagus. J Pediatr 2006; 141 (1): 77–82.
Acknowledgements
We express our gratitude to (1) Dr Raymond G Hoffmann, PhD, Department of Biostatistics, Medical College of Wisconsin, for statistical advice; (2) Dr P Sasidharan, MD, and Dr Robert M Kliegman, MD, Section of Neonatology, Department of Pediatrics, Medical College of Wisconsin for their insightful advice, guidance and support for this initiative. This work is supported in part by grant PO1 DK 068051(Jadcherla/Shaker).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Jadcherla, S., Wang, M., Vijayapal, A. et al. Impact of prematurity and co-morbidities on feeding milestones in neonates: a retrospective study. J Perinatol 30, 201–208 (2010). https://doi.org/10.1038/jp.2009.149
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2009.149
Keywords
This article is cited by
-
A decade of evidence: standardized feeding initiative targeting feeding milestones and predicting NICU stays in premature infants in an all-referral level IV NICU
Journal of Perinatology (2023)
-
Testing and Development of Slightly Thick Infant Formula Recipes for Dysphagia Management: An Australian Perspective
Dysphagia (2023)
-
Body adiposity and oral feeding outcomes in infants: a pilot study
Journal of Perinatology (2021)
-
Oral-feeding guidelines for preterm neonates in the NICU: a scoping review
Journal of Perinatology (2021)
-
A cross-sectional analysis of infant-driven and traditional feeding outcomes for neonatal intensive care unit infants
Journal of Perinatology (2021)