Abstract
Objective:
We critically reviewed every NICU blood component transfusion (packed erythrocytes, platelets, frozen plasma (FP) and cryoprecipitate) administered during a one-year period. This was done to determine the proportion of transfusions given out of compliance with the Intermountain Healthcare transfusion guidelines, and to look for patterns of non-compliance that could be addressed by quality improvement measures.
Study Design:
A detailed review was made of every transfusion administered to patients with a date of birth of 1 January 2006 through 31 December 2006, in any of three level III, perinatal-center-associated NICUs within Intermountain Healthcare.
Result:
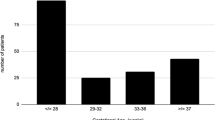
During 2006 the three NICUs cared for 1759 neonates. Seventeen percent of these received one or more (median 3) erythrocyte transfusions, 4% received one or more (median 3) platelet transfusions, 6% received one or more (median 1) FP infusions and 2% received cryoprecipitate (median 1 dose). Seventy percent of the erythrocyte transfusions were given in compliance with the guidelines, as were 69% of the platelet transfusions, 65% of the FP transfusions and 94% of the cryoprecipitate administrations. Patients who received large numbers of transfusions were more likely to receive transfusion that violated the guidelines. Forty-five percent of patients who received 1 to 3 transfusions received all transfusions within guidelines. However, only 18% of patients who received 4 to 10 transfusions received all within guidelines. No patient who received >10 transfusions received all within the guidelines. Erythrocyte transfusions given early in the hospital course were likely to be within guidelines; 72% (588/818) in the first 29 days were compliant with guidelines, but compliance fell to 61% (144/237) for transfusions administered after 29 days (P=0.002). About half of the platelet transfusions given early in the hospital course were in violation of guidelines, but after day 9, 83% of platelet transfusions were compliant with guidelines (P=0.000).
Conclusion:
Opportunities exist in our healthcare system to improve compliance with our transfusion guidelines. Such opportunities are greatest among neonates receiving multiple transfusions, among those receiving erythrocyte transfusions late in their NICU course and among those receiving platelet transfusions early in their NICU course.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Murray NA, Roberts IAG . Neonatal transfusion practice. Arch Dis Child Fetal Neonatal Ed 2004; 89: 101–107.
Luban NLC . Transfusion of blood and blood products. In: MG MacDonald, J Ramasethu (eds). Atlas of Procedures in Neonatology, 4th edn. Lippincott/Williams & Wilkins: Philadelphia, 2007, pp 317–328.
Del Vecchio A, Sola MC, Teriaque DW, Hutson AD, Kao KJ, Wright D et al. Platelet transfusions in the neonatal intensive care unit: factors predicting patients who will require multiple transfusions. Transfusion 2001; 41: 803–808.
Christensen RD, Henry E, Wiedmeier SE, Stoddard RA, Sola-Visner MC, Lambert DK et al. Thrombocytopenia among extremely-low birth-weight neonates: data from a multihospital healthcare system. J Perinatol 2006; 26: 348–353.
Kopko PM, Holland PV . Mechanisms of severe transfusion reactions. Elsevier Science, Paris 2001; 8: 278–281.
Baer VL, Lambert DK, Henry E, Snow GL, Sola-Visner MC, Christensen RD . Do platelet transfusions in the NICU adversely effect survival? Analysis of 1600 thrombocytopenic neonates in a multihospital healthcare system. J Perinatol 2007; 27: 790–796.
Sanchez R, Toy P . Transfusion related acute lung injury: a pediatric perspective. Pediatr Blood Cancer 2005; 45: 248–255.
Strauss RG . Data-driven blood banking practices for neonatal RBC transfusions. Transfusion 2000; 40: 1528–1540.
Birenbaum HJ, Pane MA, Helou SM, Starr KP . Comparison of a restricted transfusion schedule with erythropoietin therapy versus a restricted transfusion schedule alone in very low birth weight premature infants. Sout Med Journ 2006; 99: 1059–1062.
Maier RF, Sonntag J, Walka MM, Liu G, Metze BC, Obladen M . Changing practices of red blood cell transfusions in infants with birth weights less than 1000 g. J Pediatr 2000; 136: 220–224.
Miyashiro AM, Santos N, Guinsburg BI, Kopelman D, Peres DA, Taga MF et al. Strict red blood cell transfusion guideline reduces the need for transfusions in very-low-birthweight infants in the first 4 weeks of life: a multicentre trial. Vox Sang 2005; 88: 107–113.
Calhoun DA, Christensen RD, Edstrom CS, Juul SE, Ohls RK, Schibler KR et al. Consistent approaches to procedures and practices in neonatal hematology. Clin Perinatol 2000; 27: 733–753.
Venâncio JP, Santos AM, Guinsburg R, Peres Cde A, Shinzato AR, Lora MI . Strict guideline reduces the need for RBC transfusions in premature infants. J Trop Pediatr 2007; 53: 78–82.
Sola MC . Evaluation and treatment of severe and prolonged thrombocytopenia in neonates. Clin Perinatol 2004; 31: 1–14.
Hume H, Blanchette V, Strauss RG, Levy GJ . A survey of Canadian neonatal blood transfusion practices. Transfus Sci 1997; 18: 71–80.
Ringer SA, Richardson DK, Sacher RA, Keszler M, Churchill WH . Variations in transfusion practice in neonatal intensive care. Pediatrics 1998; 101: 194–200.
Petaja J, Andersson S, Syrjala M . A simple automatized audit system for following and managing practices of platelet and plasma transfusions in a neonatal intensive care unit. Transf Med 2004; 4: 281–288.
Garcia MG, Duenas E, Sola MC, Hutson AD, Theriaque D, Christensen RD . Epidemiologic and outcome studies of patients who received platelet transfusions in the neonatal intensive care unit. J Perinatol 2001; 21: 415–420.
Chevuru SC, Sola MC, Theriaque DW, Hutson AD, Leung WC, Perez JA et al. Multicenter analysis of platelet transfusion usage among neonates on extracorporeal membrane oxygenation. Pediatrics 2002; 109: e89.
Bell EF, Strauss RG, Widness JA, Mahoney LT, Mock DM, Seward VJ et al. Randomized trial of liberal versus restrictive guidelines for red blood cell transfusion in preterm infants. Pediatrics 2005; 115: 1685–1691.
Stanworth SJ . The Evidence-Based use of FFP and Cryoprecipitate for Abnormalities of Coagulation Tests and Clinical Coagulopathy. Hematology Am Soc Hematol Educ Program 2007; 2007: 179–186.
Stanworth SJ, Brunskill SJ, Hyde CJ, Murphy MF, McClelland DB . Appraisal of the evidence for the clinical use of FP and plasma fractions. Best Pract Res Clin Haematol 2006; 19: 67–82.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website (http://www.nature.com/jp)
Supplementary information
Rights and permissions
About this article
Cite this article
Baer, V., Lambert, D., Schmutz, N. et al. Adherence to NICU transfusion guidelines: data from a multihospital healthcare system. J Perinatol 28, 492–497 (2008). https://doi.org/10.1038/jp.2008.23
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2008.23
Keywords
This article is cited by
-
Fresh frozen plasma and cryoprecipitate: Can we safely reduce their use in the NICU?
Journal of Perinatology (2023)
-
Role of platelets in neonatal necrotizing enterocolitis
Pediatric Research (2021)
-
Why do four NICUs using identical RBC transfusion guidelines have different gestational age-adjusted RBC transfusion rates?
Journal of Perinatology (2015)
-
Neonates presenting with bloody stools and eosinophilia can progress to two different types of necrotizing enterocolitis
Journal of Perinatology (2012)
-
Very low birth weight infants qualifying for a ‘late’ erythrocyte transfusion: Does giving darbepoetin along with the transfusion counteract the transfusion's erythropoietic suppression?
Journal of Perinatology (2011)