Abstract
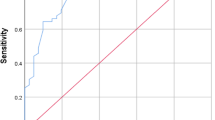
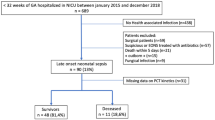
Diagnostic of early-onset neonatal infection (EONI) remains an emergency. Recent studies underline the potential benefit of using Procalcitonin (PCT) in early diagnosis of bacterial infections in neonates. The aim of this study was to evaluate the diagnostic value of an umbilical blood cord PCT based algorithm in newborns suspected of EONI. The diagnostic value of the PCT based algorithm was compared to the French one currently in use by analyzing an 18-months database of newborns suspected of EONI in University Hospital of Nantes from March 2011 to September 2012. Among the 2,408 (40.8 %) newborns suspected of infection during this period, 2,366 were included in the study. The incidence of EONI was 3.4‰ (n = 20). There was no significant difference between the sensibilities of the PCT based algorithm and the current algorithm (90 %, respectively, 95%CI 76.9–100 versus 85.4–100; p = 0.90) and between their specificities (respectively 91.7 % (90.6–92.8) versus 87.4 % (86–88.7); p = 0.25). The antibiotic treatment rate would be significantly reduced with the PCT based algorithm [211 i.e. 8.9 % (7.8–10) versus 314 i.e. 13.3 % (11.9–14.7) in the current algorithm; p < 0.005] and less biological analysis would be performed [301 i.e. 12.7 % (11.4–14) versus 937 i.e. 39.6 % (37.6–41.6); p < 0.005]. Blood cord PCT seems to be a new and efficient marker to guide neonatologists taking care of newborns suspected of EONI. The PCT algorithm seems to be a safe alternative in diagnosis of EONI, allowing detection of EONI significantly as well as the current algorithm, without resulting in a substantially higher number of missed infections. These results have to be confirmed by a multicentric validation study.



Similar content being viewed by others
References
Edmond K, Zaidi A (2010) New approaches to preventing, diagnosing, and treating neonatal sepsis. PLoS Med 7(3):e1000213
Seale AC, Mwaniki M, Newton CR, Berkley JA (2009) Maternal and early onset neonatal bacterial sepsis: burden and strategies for prevention in sub-Saharan Africa. Lancet Infect Dis 9(7):428–438
Koenig JM, Keenan WJ (2009) Group B streptococcus and early-onset sepsis in the era of maternal prophylaxis. Pediatr Clin N Am 56(3):689–708
CDC (2009) Trends in perinatal group B streptococcal disease—United States, 2000–2006. MMWR 58(5):109–112
Schrag S, Gorwitz R, Schuchat A (2002) Prevention of perinatal group B streptococcal disease. Revised guidelines from CDC. MMWR Recomm Rep 51(RR-11):1–22
Verani JR, McGee L, Schrag SJ (2010) Prevention of perinatal group B streptococcal disease—revised guidelines from CDC. MMWR Recomm Rep 59(RR-10):1–36
Puopolo KM, Madoff LC, Eichenwald EC (2005) Early-onset group B streptococcal disease in the era of maternal screening. Pediatrics 115(5):1240–1246
ANAES (2001) Prévention anténatale du risque infectieux bactérien néonatal précoce. ANAES, Haute Autorité de santé, France
ANAES (2002) Diagnostic et traitement curatif de l’infection bactérienne précoce du nouveau-né. ANAES, Haute Autorité de santé, France
Marodi L (2006) Neonatal innate immunity to infectious agents. Infect Immun 74(4):1999–2006
Sadeghi K, Berger A, Langgartner M et al (2007) Immaturity of infection control in preterm and term newborns is associated with impaired toll-like receptor signaling. J Infect Dis 195(2):296–302
Polin RA, Committee on Fetus and Newborn (2012) Management of neonates with suspected or proven early-onset bacterial sepsis. Pediatrics 129(5):1006–1015
Polin RA (2003) The “ins and outs” of neonatal sepsis. J Pediatr 143(1):3–4
Buttery JP (2002) Blood cultures in newborns and children: optimizing an everyday test. Arch Dis Child Fetal Neonatal Ed 87(1):F25–F28
Didier C, Kuhn P (2012) Late-onset neonatal infections: incidences and pathogens in the era of antenatal antibiotics. Eur J Pediatr 171:681–687
Cotten CM, Taylor S, Benjamin DK Jr et al (2009) Prolonged duration of initial empirical antibiotic treatment is associated with increased rates of necrotizing enterocolitis and death for extremely low birth weight infants. Pediatrics 123(1):58–66
Neu J (2007) Perinatal and neonatal manipulation of the intestinal microbiome: a note of caution. Nutr Rev 65(6 Pt 1):282–285
Penders J, Thijs C, van den Brandt PA et al (2007) Gut microbiota composition and development of atopic manifestations in infancy: the KOALA Birth Cohort Study. Gut 56(5):661–667
Russell SL, Finlay BB (2012) Early life antibiotic-driven changes in microbiota enhance susceptibility to allergic asthma. EMBO Rep, Canada
Schuetz P, Christ-Crain M, Thomann R et al (2009) Effect of procalcitonin-based guidelines vs standard guidelines on antibiotic use in lower respiratory tract infections: the ProHOSP randomized controlled trial. JAMA 302(10):1059–1066
Berg P, Lindhardt BØ (2012) The role of procalcitonin in adult patients with community-acquired pneumonia—a systematic review. Dan Med J 59(3):A4357
Maniaci V, Dauber A, Weiss S et al (2008) Procalcitonin in young febrile infants for the detection of serious bacterial infections. Pediatrics 122(4):701–710
Fioretto JR, Borin FC, Bonatto RC et al (2007) Procalcitonin in children with sepsis and septic shock. J Pediatr (Rio J) 83(4):323–328
Gomez B, Bressan S et al (2012) Diagnostic value of procalcitonin in well-appearing young febrile infants. Pediatrics 130(5):815–822
Simon L, Gauvin F, Amre DK et al (2004) Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: a systematic review and meta-analysis. Clin Infect Dis 39(2):206–217
Gendrel D, Assicot M, Raymond J et al (1996) Procalcitonin as a marker for the early diagnosis of neonatal infection. J Pediatr 128(4):570–573
Van Rossum AM, Wulkan RW, Oudesluys-Murphy AM (2004) Procalcitonin as an early marker of infection in neonates and children. Lancet Infect Dis 4(10):620–630
Vouloumanou EK, Plessa E, Karageorgopoulos DE et al (2011) Serum procalcitonin as a diagnostic marker for neonatal sepsis: a systematic review and meta-analysis. Intensive Care Med 37(5):747–762
Chiesa C, Pellegrini G et al (2003) C-reactive protein, interleukin-6, and procalcitonin in the immediate postnatal period: influence of illness severity, risk status, antenatal and perinatal complications, and infection. Clin Chem 49(1):60–68
Vazzalwar R, Pina-Rodrigues E, Puppala BL et al (2005) Procalcitonin as a screening test for late-onset sepsis in preterm very low birth weight infants. J Perinatol 25(6):397–402
Turner D, Hammerman C, Rudensky B et al (2006) Procalcitonin in preterm infants during the first few days of life: introducing an age related nomogram. Arch Dis Child Fetal Neonatal Ed 91(4):F283–F286
Lopez Sastre JB, Solis DP, Serradilla VR et al (2007) Evaluation of procalcitonin for diagnosis of neonatal sepsis of vertical transmission. BMC Pediatr 7:9
Chiesa C, Panero A, Rossi N et al (1998) Reliability of procalcitonin concentrations for the diagnosis of sepsis in critically ill neonates. Clin Infect Dis 26(3):664–672
Joram N, Muller JB, Denizot S (2011) Umbilical cord blood procalcitonin level in early neonatal infections: a 4-year university hospital cohort study. Eur J Clin Microbiol Infect Dis 30:1005–1013
Joram N, Boscher C, Denizot S et al (2006) Umbilical cord blood procalcitonin and C reactive protein concentrations as markers for early diagnosis of very early onset neonatal infection. Arch Dis Child Fetal Neonatal Ed 91(1):F65–F66
Kordek A, Hałasa M, Podraza W (2008) Early detection of an early onset infection in the neonate based on measurements of procalcitonin and C-reactive protein concentrations in cord blood. Clin Chem Lab Med 46(8):1143–1148
National Collaborating Centre for Women's and Children's Health (UK) (2012) Antibiotics for early-onset neonatal infection. National Institute for Health and Clinical Excellence, RCOG Press, London
Haque KN (2005) Definitions of bloodstream infection in the newborn. Pediatr Crit Care Med 6(3 Suppl):S45–S49
Hofer N, Müller W, Resch B (2011) Non-infectious conditions and gestational age influence C-reactive protein values in newborns during the first 3 days of life. Clin Chem Lab Med 49(2):297–302
Mims LC, Medawar MS, Grubb WR et al (1972) Predicting neonatal infections by evaluation of the gastric aspirate: a study in two hundred and seven patients. Am J Obstet Gynecol 114(2):232–238
Competing interest
None declared.
Funding statement
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Contributorship statement
S. Lencot, B. Cabaret, G. Sauvage and C. Laurans monitored data collection for the whole trial; S. Lencot analyzed the data, wrote the statistical analysis plan and drafted the paper. C. Gras-Leguen initiated the collaborative project, implemented the trial in the hospital, designed data collection tools and revised the paper; she is the guarantor. J-C. Rozé, J. Caillon, J-L. Orsonneau, C. Boscher and E. Launay revised the draft paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
What is already known on this topic:
Clinical symptoms and biological markers are neither sensitive nor specific for the diagnosis of early-onset neonatal infection. Recent studies underline the benefit of Procalcitonin in bacterial infections.
What this study adds:
The study showed that an algorithm based on cord Procalcitonin would have an interesting diagnostic value and would allow performing less blood tests and less antibiotics treatments.
Rights and permissions
About this article
Cite this article
Lencot, S., Cabaret, B., Sauvage, G. et al. A new procalcitonin cord-based algorithm in early-onset neonatal infection: for a change of paradigm. Eur J Clin Microbiol Infect Dis 33, 1229–1238 (2014). https://doi.org/10.1007/s10096-014-2065-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-014-2065-3