Abstract
Introduction
Hypothermia at birth is strongly associated with mortality and morbidity in pre-term infants.
Background
A local audit showed limited effectiveness of occlusive wrapping in preventing admission hypothermia in very pre-term infants. Self-heating acetate gel mattresses were introduced as a result to prevent hypothermia at birth in infants born at or below 28 weeks gestation.
Methods
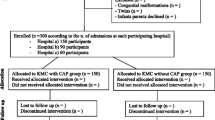
A retrospective audit was conducted to evaluate the effectiveness of self-heating acetate gel mattresses at resuscitation of infants born at or below 28 weeks to prevent hypothermia at birth. All infants born at or below 28 weeks gestation during 18 months before and 18 months after self-heating acetate gel mattresses were introduced during resuscitation were included.
Results
One hundred five babies were born when acetate gel mattresses were not used, and 124 were born during the period when they were. Four (3.3%) babies were hypothermic (temperature <36°C) at admission when the mattresses were used compared to 21 (22.6%) babies who were hypothermic during the period it was not (p < 0.001). Hyperthermia (temperature >37°C) rose from 30.1% prior to use of gel mattresses to 49.6% when they were used (p = 0.004).
Conclusions
Self-heating acetate gel mattresses are highly effective in reducing admission hypothermia in infants born at or below 28 weeks gestation. The use of these mattresses is associated with a significant increase in hyperthermia.


Similar content being viewed by others
References
Bergman NJ, Linley LL, Fawcus SR (2004) Randomized controlled trial of skin-to-skin contact from birth versus conventional incubator for physiological stabilization in 1200- to 2199-gram newborns. Acta Paediatr 93:779–785
Carmichael A, McCullough S, Kempley ST (2007) Critical dependence of acetate thermal mattress on gel activation temperature. Arch Dis Child Fetal Neonatal Ed 92:F44–F45
Chaput de Saintonge DM, Cross KW, Shathorn MK, Lewis SR et al (1979) Hats for the newborn infant. Br Med J 2:570–571
Confidential Enquiry into Stillbirths and Deaths in Infancy (2003) PROJECT 27/28, an enquiry into quality of care and its effect on the survival of babies born at 27–28 weeks. Maternal and Child Health Research Consortium, London
Costeloe K, Hennessy E, Gibson AT, Marlow N et al (2000) The EPICure study: outcomes to discharge from hospital for infants born at the threshold of viability. Pediatrics 106:659–671
Craig JV, Lancaster GA, Williamson PR, Smyth RL (2000) Temperature measured at the axilla compared with rectum in children and young people: systematic review. Br Med J 320:1174–1178
Falzon A, Grech V, Caruana B, Magro A et al (2003) How reliable is axillary temperature measurement? Acta Paediatr 92:309–313
Ibrahim CPH, Yoxall CW (2009) Use of plastic bags to prevent hypothermia at birth in preterm infants—do they work at lower gestations? Acta Paedtr 98:256–260
Knobel RB, Wimmer JE Jr, Holbert D (2005) Heat loss prevention for preterm infants in the delivery room. J Perinatol 25:304–308
L'Herault J, Petroff L, Jeffrey J (2001) The effectiveness of a thermal mattress in stabilizing and maintaining body temperature during the transport of very low-birth weight newborns. Appl Nurs Res 14:210–219
Lofgren O, Jacobson L (1979) The influence of different electrode temperatures on recorded transcutaneous pO2 level. Pediatrics 64:892–897
Mathew B, Lakshminrusimha S, Cominsky K, Schroder E et al (2007) Vinyl bags prevent hypothermia at birth in preterm infants. Indian J Pediatr 74:249–253
McCall EM, Alderdice FA, Halliday HL, Jenkins JG et al (2008) Interventions to prevent hypothermia at birth in preterm and/or low birthweight infants. Cochrane Database of Systematic Reviews 2008, Issue 1. Art. No.: CD004210. doi:10.1002/14651858.CD004210.pub3
Vohra S, Frent G, Campbell V, Abbott M et al (1999) Effect of polyethylene occlusive skin wrapping on heat loss in very low birth weight infants at delivery: a randomized trial. J Pediatr 134:547–551
Vohra S, Roberts RS, Zhang B, Janes M et al (2004) Heat Loss Prevention (HeLP) in the delivery room: a randomized controlled trial of polyethylene occlusive skin wrapping in very preterm infants. J Pediatr 145:750–753
Wang W, Dow KE, Flavin MP (2008) Hyperthermia amplifies brain cytokine and reactive oxygen species response in a model of perinatal inflammation. Neurosci Lett 445:233–235
Watkinson M (2006) Temperature control of premature infants in the delivery room. Clin Perinatol 33:43–53
Competing interests
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ibrahim, C.P.H., Yoxall, C.W. Use of self-heating gel mattresses eliminates admission hypothermia in infants born below 28 weeks gestation. Eur J Pediatr 169, 795–799 (2010). https://doi.org/10.1007/s00431-009-1113-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-009-1113-y