Abstract
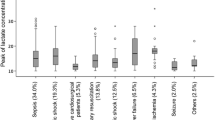
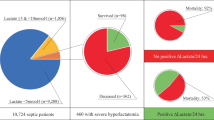
Objective: To examine the relationships between early hyperlactataemia, acidosis, organ failure, and mortality in children admitted to intensive care.¶Design: Prospective observational study. Children with lactate levels > 2 mmol/l were eligible for enrolment. Post-operative patients and those with inherited metabolic disease were excluded. Seven hundred and five children admitted to intensive care were screened, and 50 children with hyperlactataemia (incidence 7 %), aged 20.3 months (0.1–191) were enrolled and followed up. The Paediatric Risk of Mortality (PRISM) score, Multiorgan System Failure (MOSF) score, length of ICU stay, and outcome were recorded. Data were collected for lactate (mmol/l), pH, and base excess (BE) until 24 h after admission. Data are reported as median (range) and were analysed by the Mann-Whitney, Fisher's Exact, and Kruskal-Wallis tests, and chi-squared test for trend.¶Results: Overall mortality in the screening group was 70/705 (10 %). In the study group (n = 50) median PRISM score was 19 (4–49), median MOSF score 2 (1–4), and observed mortality 32/50 (64 %). Median duration of ICU stay was 6 days (2–32) in survivors, and median time until death 3 days (0–13) in nonsurvivors. Eleven nonsurvivors (34 %) died within 24 h. In the screening group, hyperlactataemia on admission identified mortality with likelihood ratio = 15. In the study group, neither the admission lactate (3.8 vs 4.6 mmol/l, P = 0.27), pH (7.32 vs 7.30, P = 0.6), nor BE (–7.5 vs –8, P = 0.45) differed significantly between survivors and nonsurvivors. Neither the admission nor peak lactate increased with increasing MOSF score (P = 0.5 and 0.54). The median peak lactate level was 5 mmol/l (2–9.3) in survivors compared to 6.8 mmol/l (2.3–22) in nonsurvivors (P = 0.02), and the cumulative average lactate level was 2.4 mmol/l (1–4.9) in survivors, compared to 4.5 mmol/l (1.6–21) in nonsurvivors (P = 0.0003). Persistent hyperlactataemia 24 h after admission identified mortality with likelihood ratio = 7.¶Conclusion: Hyperlactataemia on admission to intensive care is associated with a high mortality in children. Nonsurvivors within this group may be distinguished by the peak lactate level, or by persistent hyperlactataemia after 24 h of treatment.
Similar content being viewed by others
Author information
Authors and Affiliations
Additional information
Received: 2 July 1999/Final revision received: 2 July 1999/Accepted: 30 November 1999
Rights and permissions
About this article
Cite this article
Hatherill, M., McIntyre, A., Wattie, M. et al. Early hyperlactataemia in critically ill children. Intensive Care Med 26, 314–318 (2000). https://doi.org/10.1007/s001340051155
Issue Date:
DOI: https://doi.org/10.1007/s001340051155