Abstract
Objective
To test the hypothesis in ventilated very low birth weight infants with frequent hypoxemic episodes that volume-controlled synchronized intermittent mandatory ventilation (SIMV) vs. pressure-controlled SIMV reduces by at least 20% the time with hypoxemia (defined as SpO2< 80%).
Design
Randomized cross-over design.
Setting
University-based tertiary neonatal intensive care unit.
Patients
15 mechanically ventilated very low birth weight infants with frequent hypoxemic episodes.
Interventions
The infants were exposed in random order to volume-controlled and pressure-controlled SIMV for 4 h each. The target tidal volume during volume-controlled SIMV was matched to the tidal volume measured during pressure-controlled SIMV. FIO2 was adjusted using uniform criteria to maintain SpO2 within the target range (SpO2 80–92%).
Measurements and results
Primary outcome measure was the time with an SpO2< 80%. Although tidal volume was maintained better during desaturations with volume-controlled SIMV, there was neither a significant difference in time with an SpO2< 80% (expressed as proportion of total experimental time; median, interquartile range)—volume-control 10.6% (9.2–13.7%) vs. pressure-control 10.8% (8.3–13.3%)—nor in FIO2 exposure. During volume-controlled SIMV the infants spent less time with an SpO2 above the target range and had fewer associated bradycardias.
Conclusion
Volume-controlled SIMV did not decrease the time with an SpO2< 80%, although tidal volume was better maintained during these episodes and bradycardias were less frequent than with pressure-controlled SIMV in this population of very low birth weight infants with frequent hypoxemic episodes.
Similar content being viewed by others
Introduction
Preterm infants undergoing mechanical ventilation often present with episodes of hypoxemia [1]. Although the pathophysiology of these episodes is not entirely understood, the rapid onset of hypoxemia observed in small infants with hypoxemic episodes suggests that intrapulmonary shunting may play a significant role [2]. A substantial number of hypoxemic episodes do not seem to be related to apnea and thereby hypoventilation but rather may be caused by active exhalation despite presence of positive end-expiratory pressure (PEEP), resulting in loss of functional residual capacity (FRC) and increased intrapulmonary shunting [3]. These events are associated with a drop in compliance and increased resistance suggesting that the closing volume of some lung units is reached [3]. This proposed mechanism explains the rapid onset of hypoxemia secondary to intrapulmonary shunts. Use of a volume-controlled (VC) rather than a pressure-controlled (PC) mechanical ventilator may prevent the decrease in FRC during these episodes or may allow automatic recruitment of collapsed lung units faster, as the driving pressure is increased automatically. Therefore we hypothesized that the time with hypoxemia (defined as arterial oxygen saturation as measured by pulse oximetry, SpO2, less than 80%) is at least 20% less with VC than with PC synchronized intermittent mandatory ventilation (SIMV)2 in very low birth weight infants with hypoxemic episodes.
Methods
Patients
Subjects eligible to enter this study were endotracheally intubated infants (birthweight < 1500 g) with at least ten mechanical breaths/min and at least two episodes/h of desaturation, defined as SpO2 less than 75% for at least 8 h within the preceding 24 h. The episodes of desaturation were confirmed using a Radical pulse oximeter (Masimo, Irvine, Calif., USA). The study was approved by the ethics committee for the protection of human subjects of the University of Ulm, and informed written consent was obtained from the parents of each of the study infants. Infants with congenital malformations, an endotracheal tube leak of more than 20% as measured by the pneumotachograph of the mechanical ventilator, and a peak inspiratory pressure greater than 22 cmH2O were excluded from the study because the maximal relative increase in airway pressure during VC SIMV would have been smaller as the upper pressure limit was set to 40 cmH2O.
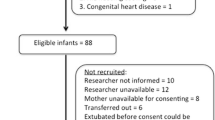
Twenty-one ventilated preterm infants were screened with pulse oximetry recordings to check for eligibility. Four were not eligible to enter the study because they did not have at least two episodes/h of desaturation for at least 8 h, one because of a large leak around the endotracheal tube, and one for being scheduled for ligation of a persistent ductus arteriosus. The remaining 15 study infants had a birth weight of 612 ± 149 g and a gestational age of 24.8 ± 1.6 weeks. The infants were on mechanical ventilation at study time because of limited respiratory drive and/or a mild or moderate degree of respiratory failure, but were otherwise stable. They were studied at a postnatal age of 33 ± 13 days and their weight at study time was 937 ± 264 g.
Mechanical ventilator
A Stephanie infant ventilator (Stephan Medizintechnik, Gackenbach, Germany) was used, which is equipped with a very fast selenoid valve and a pneumotachograph. In addition to the usual pressure controlled mode, it can provide true VC-SIMV, i.e., it increases the ventilator pressure within each breath if necessary based on the inspiratory flow measured, to reach the desired tidal volume at the end of the inspiratory time chosen (response time 10 ms). All study infants had been on time-cycled PC mechanical ventilation (with variable flow for leak compensation) before the study, and the ventilator settings chosen by the clinical team at study time were: FIO2: 0.35 ± 0.12, peak inspiratory pressure: 19.7 ± 1.3 cmH2O, inspiratory time: 0.37 ± 0.06 s, PEEP: 5–6 cmH2O with a ventilator rate of 39 ± 13 breaths/min. These settings remained unchanged during the study except for adjustments described in the study design.
Study design
A randomized cross-over design was used. The infants were exposed in random order (sealed envelopes) for 4 h each to PC SIMV with ventilatory settings as chosen by the clinician taking care on the infants and to VC SIMV using a target tidal volume as measured during the ventilator settings chosen by the clinician immediately before the study. This tidal volume was 7.8 ± 1.4 ml/kg. The upper safety limit for pressure during VC SIMV was set at twice the inspiratory pressure chosen by the clinician before the study, but no more than 40 cmH2O. By these criteria the safety limit for inspiratory pressure was 36–40 cmH2O in all infants. Standardized criteria were applied during both ventilatory conditions to adjust FIO2 in relation to the SpO2 measured as follows: SpO2 80–92% (usual target range used in our neonatal ICU for preterm infants with an immature retina): no change in FIO2; SpO2 greater than 92% for more than 60 s: FIO2 was decreased by 0.05 every 60 s until target range was reached; SpO2 less than 80% for more 60 s: FIO2 was increased by 0.05 every 60 s, until target range was reached; SpO2 less than 70%: immediate increase in FIO2 by increments 0.1 every 30 s; SpO2 less than 60%: immediate increase in FIO2 by increments of 0.2 every 30 s; SpO2 less than 50%: immediate increase in FIO2 to 1.0. These adjustments were performed by dedicated research personnel using a stop-watch and present at bedside throughout study time. All infants were studied in supine position during both modes. Other procedures in patient care (i.e., feeding or suctioning) were performed by the nursing staff, who were not allowed to adjust any ventilatory setting during the study. Timing of the study was scheduled to not interfere with nursing rounds, i.e., nursing rounds were carried out immediately before or after each of the two 4-h study periods. No sedation was given during study time.
Measurements
SpO2 and the plethysmography curve of the pulse oximeter and electrocardiography was recorded with an IVY monitor Model 405T (IVY Medical Systems, Branford, Conn., USA), equipped with an LNOP-Neo Sensor. This device is equipped with Masimo signal extraction technique (Masimo SET, Masimo, Irvine, Calif., USA), which has been shown to be associated with less motion artifacts than other systems available [4]. FIO2 was measured with the sensor device of the ventilator. Transcutaneous PCO2 was measured using a Tina (Radiometer, Copenhagen, Denmark) which was calibrated immediately before each of the two study periods. Air flow was measured with the pneumotachograph, which was placed between the ventilator circuit and the endotracheal tube. Airway and esophageal pressure were measured using Sorensen Transpac 4 sensors (Abbott Critical Care Systems, North Chicago, Ill., USA). The heart rate was obtained from the electrocardiographic signal from the IVY monitor. All signals were digitized and recorded continuously with a sample rate of 100 Hz on a computer system.
Data analysis and statistics
The primary outcome measure was the total time with an SpO2 less than 80%. Secondary outcome measures were the total time with SpO2 above and the total time with an SpO2 within the target range (80–92%), incidence and duration of episodes of desaturation (defined as SpO2 less than 80%), lowest SpO2 (trough) during each of these episodes, incidence of bradycardia (defined as a heart rate below 100/min), FIO2 exposure, and number of changes in FIO2 necessary to maintain the SpO2 target range. Furthermore, changes in tidal volume, lung compliance and resistance, based on trans-pulmonary pressure measurements and analyzed as described previously [5], tracheal leak, and airway pressure during the five episodes with the lowest trough in SpO2 with each ventilatory mode in each infant were measured to further characterize the episodes of desaturation.
Paired data were compared using the paired t test or Wilcoxon signed rank test, where appropriate. Differences with p values less than 0.05 were considered statistically significant. We were unable to perform a sample size calculation because the variance of the primary outcome measure was unknown. Therefore we decided to use a study design with an integrated pilot sample of 15 babies and to perform an adaptive interim analysis thereafter [6]. Values presented are medians and interquartile ranges (25th–75th percentiles) unless stated otherwise.
Results
Our hypothesis the time with hypoxemia (defined as SpO2 less than 80%) is less during VC SIMV than during PC SIMV was not confirmed. There was no significant difference in time with hypoxemia (Table 1). Figure 1 shows the individual values for each infant during both ventilatory conditions. During VC SIMV the infants spent significantly less time with an SpO2 above the target range (SpO2 > 92%) than during PC SIMV (20%, 14.6–23.2%, vs. 25.9%, 16.6–31.0%; p = 0.04; Fig. 2). Furthermore, there was a trend towards more time spent within the SpO2 target range during VC (70.7%, 62.8–78.7%) than during PC (62.2%, 54.6–75.6%); p = 0.09). Although there was a trend towards more exposure to an FIO2 of 0.7–1.0 when analyzed as timely exposure to different FIO2 categories during PC SIMV (Fig. 3), the average FIO2 used during the complete experimental period did not differ between modes (Table 3).
Table 1 shows characteristics of the episodes of desaturations for both ventilator modes. There was no difference in the number of desaturations comparing the two ventilatory modes. Most episodes were associated with an increase in esophageal pressure within 30 s before the onset of hypoxemia during both ventilatory modes. There was a trend towards lower troughs in SpO2 during episodes of desaturation during PC SIMV. There was no significant difference in the median duration of the episodes. However, the number of associated bradycardias was lower during VC than during PC SIMV, and there was a trend toward a lower number of standardized FIO2 adjustments necessary to maintain SpO2 within the target range.
Table 2 shows pulmonary function parameters immediately before and during the five episodes with the lowest trough in SpO2 with each ventilatory mode. During the episodes of desaturation tidal volume was maintained better in the VC mode, whereas there was no detectable difference in air leak between modes. There was a trend toward a lower lung compliance during PC than during VC mode, suggesting that more distal lung units were collapsed during the episodes when using PC mode. Comparing individual lung compliance values before desaturations with values during desaturations we found a larger decline in lung compliance with PC than with VC SIMV. As expected, the driving airway pressure above PEEP increased during the episodes during VC SIMV, whereas there was no change in PC mode.
Figure 4 shows typical examples of hypoxemic episodes during both ventilatory conditions with desaturations immediately preceded by a rise in esophageal pressure, suggesting increased thoracic pressure. During both ventilatory modes the increase in intrathoracic pressure resulted in an immediate decrease in FRC, as suggested by the transient downward shift of the tidal volume trace. The rapid decline in FRC explains the sudden drop in SpO2 after a few seconds. Although tidal flow and tidal volume was maintained better during VC than during PC SIMV, the shift of the volume trace was not prevented.
Air flow, tidal volume, esophageal (Pe) and airway pressure (Paw), oxygen saturation (SpO 2), and heart rate of the same infant during during pressure-controlled SIMV (upper panel) and volume-controlled SIMV (lower panel). During both ventilatory modes the increase in intrathoracic pressure indicated by the rise in Pe (asterisk) resulted in an immediate loss in functional residual capacity (FRC), as can be seen in the transient downward shift of the tidal volume trace (arrow). This rapid decline in FRC explains the sudden drop in SpO2 after a few seconds (filled triangle). Note: Tidal flow and tidal volume are maintained better during VC than during PC SIMV. However, this does not prevent the loss in FRC
When averaged across the 4-h experimental period, there were no differences between VC and PC modes in mean airway pressure, minute ventilation, respiratory rate, tidal volume, FIO2 exposure, SpO2, PCO2, or heart rate (Table 3).
Discussion
Our findings confirm those of Bolivar and coworkers [3] who reported that most episodes of hypoxemia in preterm infants undergoing mechanical ventilation are triggered by a forced expiratory effort resulting in a decrease in FRC. We found that close to 90% of all episodes of desaturation were preceded by an increase in esophageal pressure, indicating a rise in pleural pressure, which suggests the occurrence of a forced expiratory effort. Further, we found a decreased lung compliance and increased resistance of the respiratory system, suggesting distal airway closure and alveolar collapse [7].
However, our VC SIMV approach did not reduce the total time with an SpO2 less than 80%. This may be related to increased leak around the endotracheal tube once the VC ventilator increases the pressure to maintain tidal volume. However, we did not observe a substantial increase in endotracheal leak. On the other hand, the tight guidelines used for adjusting FIO2 may have obscured real changes in SpO2. Furthermore, mechanisms, other than active exhalation may be responsible for some of the episodes of hypoxemia in our infants. We did not measure FRC to confirm the proposed loss in FRC as the key mechanism during these episodes, but the transient downward shift in volume trace (Fig. 4) is highly suggestive. Various sleep states [8] have been found to be associated with hypoxemic episodes [9]. We did not evaluate sleep states systematically in our study, but it was our impression that there was an association of subtle body movements and with the onset of many hypoxemic episodes, as described before by others [10].
Increasing the upper pressure limit would not change results as it was reached only during a minority of episodes of desaturation during VC SIMV. Our VC mode was able to maintain tidal volume and resulted in a smaller decline in lung compliance during the episodes of desaturation but apparently did not help to maintain FRC sufficiently enough to prevent a clinically significant decline in SpO2.
Although we could not confirm that VC SIMV reduces the number of hypoxemic episodes, it may have some effect on the lowest SpO2 and the incidence of bradycardias during the episodes of desaturation. Using standardized intervention criteria for FIO2 adjustments, we found that the infants spent less time with an SpO2 above the target range and noted a trend towards more time spent within the target range. This observation suggests that episodes of hyperoxemia, which are often observed in clinical practice after FIO2 is increased in response to hypoxemic episodes, are more effectively attenuated using VC SIMV than hypoxemic episodes. This is further supported by the observed trend toward less exposure to an FIO2 of 0.7–1.0 during VC than during PC SIMV. Because the occurrence of retinopathy of prematurity [11] or bronchopulmonary dysplasia [12] may be related to the degree of oxygen exposure, VC SIMV may potentially reduce the incidence or severity of this morbidity by reducing oxygen exposure. However, it remains unknown whether the magnitude of the effects observed is clinically relevant. We did observe a trend toward less interventions necessary to maintain a specific SpO2 target range using uniform prespecified intervention criteria for FIO2 adjustments, suggesting that VC SIMV would reduce the workload for nurses or respiratory therapists.
Our study has several limitations. First, in comparison to other recommendations [13], we used a lower target range for SpO2 in our study infants, which has been shown to result in a higher incidence of desaturation episodes [14]. However, the optimal SpO2 target range for preterm infants is controversial [13, 15]. Furthermore, we applied the same target range during both ventilatory conditions. Therefore it seems unlikely that the main results of our study would change if a higher target range would have been used. We speculate that episodes of hyperoxemia would have been more common when using a higher target range for SpO2, and that differences in time with hyperoxemic conditions comparing the two ventilatory modes would have been more pronounced. Second, we studied preterm infants with frequent episodes of desaturation. This approach may have led to a selected population with severe spells, and it remains unknown whether a less selective group of infants with less severe spells would experience a smaller drop in FRC, which may be treated successfully with VC SIMV.
An alternative to VC ventilation may be volume-guaranteed ventilation [16], which works in a very different way, by increasing ventilator pressure based on expiratory tidal volume measurements of preceding breaths, resulting in a more gradual adjustment of ventilatory pressure over time. Recently a detailed evaluation of this ventilatory mode clearly showed that it works very well in the vast majority of inflations and identified a small proportion of breaths with “interrupted expiration” that interfere with calculation of tidal volume [17]. However, a “true” VC mode, which adjusts airway pressure within the first breath, was chosen in our study instead of a volume-targeted system, as the latter system may respond too slowly to the rapid changes in lung mechanics observed in infants with hypoxemic episodes [3].
Other interventions to reduce hypoxic episodes may be a closed-loop control of FIO2 [18] an automatic increase in the ventilator rate once minute ventilation drops below a certain threshold [19] or prone positioning, which has been shown to reduce episodes of hypoxemia in infants with chronic lung disease as compared to supine position [10, 20].
We were somewhat surprised by the relatively large tidal volume of approx. 7 ml/kg chosen by the clinicians, as we usually aim in our neonatal ICU for a tidal volume of 4–6 ml/kg. However, according to the study protocol the tidal volume measured immediately before the study had to be used.
Although our study did not show a lower incidence of desaturations during VC SIMV, long-term use of volume-targeted ventilation may have other beneficial effects as variability in tidal volume is clearly decreased, which may prevent the proinflammatory response of the lung, observed in the experimental setting by both high-tidal and low-tidal volume ventilation [21]. Although no large-scale randomized trials are available, there is evidence to suggest that volume-targeted vs. pressure-limited ventilation in neonates reduces duration of mechanical ventilation and markers of short-term morbidity, such as pneumothorax and intraventricular hemorrhage [22, 23].
We conclude that in this population of very low birth weight infants with high risk for severe desaturations tidal volume is maintained better during desaturations with VC than with PC SIMV. Furthermore, there seems to be some improvement in lung compliance during episodes of desaturation with VC SIMV. However, there was no effect on time with SpO2 less than 80% or on overall FIO2 exposure. VC SIMV resulted in fewer episodes of bradycardia and less time with an SpO2 above the target range and may reduce exposure to a high FIO2 and may potentially reduce the number of adjustments in FIO2 necessary to maintain SpO2 within a given target range. However, it remains unknown whether the magnitude of the effects of VC SIMV on hyperoxic exposure is large enough to result in a lower incidence or severity of morbidity, such as of retinopathy of prematurity or bronchopulmonary dysplasia. Randomized clinical trials are necessary to investigate whether the short-term benefits found in this and other studies translate into improved long-term outcomes.
References
Durand M, McEvoy C, MacDonald K (1992) Spontaneous desaturations in intubated very low birth weight infants with acute and chronic lung disease. Pediatr Pulmonol 13:136–142
Poets CF, Samuels MP, Southall DP (1992) Potential role of intrapulmonary shunting in the genesis of hypoxemic episodes in infants an young children. Pediatrics 90:385–391
Bolivar JM, Gerhardt T, Gonzalez A, Hummler H, Claure N, Everett R, Bancalari E (1995) Mechanisms for episodes of hypoxemia in preterm infants undergoing mechanical ventilation. J Pediatr 127:767–773
Bohnhorst B, Peter CS, Poets CF (2000) Pulse oximeters' reliability in detecting hypoxemia and bradycardia: Comparison between a conventional and two new generation oximeters. Crit Care Med 28:1565–1568
Silva Neto G, Gerhardt T, Silberberg A, Claure N, Duara S, Bancalari E (1992) Nonlinear pressure/volume relationship and measurements of lung mechanics in infants. Pediatr Pulmonol 12:146–152
Bauer B, Koehne K (1994) Evaluation of experiments with adaptive interim analyses. Biometrics 50:1029–1041
Mansell A, Bryan C, Levison H (1972) Airway closure in children. J Appl Physiol 33:711–714
Curzi-Dascalova L, Figueroa JM, Eiselt M, Christova E, Virassamy A, d'Allest AM, Guimaraes H, Gaultier C, Dehan M (1993) Sleep state organization in premature infants of less than 35 weeks' gestational age. Pediatr Res 34:624–628
Lehtonen L, Johnson MW, Bakdash T, Martin RJ, Miller MJ, Scher MS (2002) Relation of sleep state to hypoxemic episodes in ventilated extremely-low-birth-weight infants. J Pediatr 141:363–369
Dimaguila MA, Di Fiore JM, Martin RJ, Miller MJ (1997) Characteristics of hypoxemic episodes in very low birth weight infants on ventilatory support. J Pediatr 130:577–583
Flynn JT, Bancalari E, Snyder ES, Goldberg RN, Feuer W, Cassady J, Schiffman J, Feldman HI, Bachynski B, Buckley E et al (1992) A cohort study of transcutaneous oxygen tension and the incidence and severity of retinopathy of prematurity. N Engl J Med 326:1050–1054
The STOP-ROP Multicenter Study Group (2000) Supplemental therapeutic oxygen for prethreshold retinopathy of prematurity (STOP-ROP), a randomized, controlled trial. I. Primary outcomes. Pediatrics 105:295–310
Hay Jr WW, Thilo E, Curlander JB (1991) Pulse oximetry in neonatal medicine. Clin Perinatol 18:441–472
McEvoy C, Durand M, Hewlett V (1993) Episodes of spontaneous desaturations in infants with chronic lung disease at two different levels of oxygenation. Pediatr Pulmonol 15:140–144
Cole CH, Wright KW, Tarnow-Mordi W, Phelps DL, Pulse Oximetry Saturation Trial for Prevention of Retinopathy of Prematurity Planning Study Group (2003) Resolving our uncertainty about oxygen therapy. Pediatrics 112:1415–1419
Herrera CM, Gerhardt T, Claure N, Everett R, Musante G, Thomas C, Bancalari E (2002) Effects of volume-guaranteed synchronized intermittent mandatory ventilation in preterm infants recovering from respiratory failure. Pediatrics 110:529–533
McCallion N, Lau R, Dargaville PA, Morley CJ (2005) Volume guarantee ventilation, interrupted expiration, and expiratory braking. Arch Dis Child 90:865–870
Claure N, Gerhardt T, Everett R, Musante G, Herrera C, Bancalari E (2001) Closed-loop controlled inspired oxygen concentration for mechanically ventilated very low birth weight infants with frequent episodes of hypoxemia. Pediatrics 107:1120–1124
Claure N, Gerhardt T, Hummler H, Everett R, Bancalari E (1997) Computer-controlled minute ventilation in preterm infants undergoing mechanical ventilation. J Pediatr 131:910–913
McEvoy C, Mendoza ME, Bowling S, Hewlett V, Sardesai S, Durand M (1997) Prone positioning decreases episodes of hypoxemia in extremely low birth weight infants (1000 grams or less) with chronic lung disease. J Pediatr 130:305–309
Caruso P, Meireles SI, Reis LF, Mauad T, Martins MA, Deheinzelin D (2003) Low tidal volume ventilation induces proinflammatory and profibrogenic response in lungs of rats. Intensive Care Med 29:1808–1811
Sinha SK, Donn SM, Gavey J, McCarty M (1999) A randomised trial of volume-controlled versus time-cycled, pressure-limited ventilation in preterm infants with respiratory distress syndrome. Arch Dis Child 77:F202–F205
McCallion N, Davis P, Morley C (2005) Volume-targeted versus pressure-limited ventilation in the neonate. Cochrane Database Syst Rev 20:CD003666
Acknowledgements
We thank Nelson Claure, PhD, University of Miami, Florida, USA, for technical support.
Author information
Authors and Affiliations
Corresponding author
Additional information
This research was supported by the German Research Foundation (Hu 793/2-1). The IVY pulse oximeter was kindly provided by Masimo, (Irvine, Calif., USA).
Rights and permissions
About this article
Cite this article
Hummler, H.D., Engelmann, A., Pohlandt, F. et al. Volume-controlled intermittent mandatory ventilation in preterm infants with hypoxemic episodes. Intensive Care Med 32, 577–584 (2006). https://doi.org/10.1007/s00134-006-0079-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0079-8