Abstract
Objective:
To study the effects of implementing a method for surfactant administration by transient intubation, INSURE (i.e. INtubation SURfactant Extubation) during nasal continuous positive airway pressure (nCPAP) for moderately preterm infants with respiratory distress syndrome (RDS).
Study design:
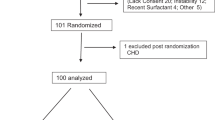
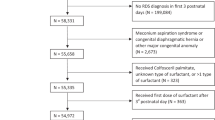
A descriptive, retrospective, bi-center study in Stockholm, Sweden, comparing mechanical ventilation (MV) rates, surfactant use, treatment response and outcome of all inborn infants with gestational age 27 to 34 weeks and RDS, (n=420), during the 5-year periods before and after the introduction of the INSURE-strategy at one of the centers (Karolinska Huddinge) in 1998. The other center (Karolinska Solna) continued conventional surfactant therapy in conjunction with MV throughout the study.
Results:
Implementation of INSURE at Karolinska Huddinge reduced the number of infants requiring MV by 50% (P<0.01), resulted in earlier surfactant administration and increased overall surfactant use. INSURE-treatment improved oxygenation and the treatment response was sustained over time with only 17% of the infants requiring >1 dose of surfactant. At Karolinska Solna, the MV rates were unaltered between the first and second 5-year period.
Conclusion:
Implementing a strategy of surfactant administration by transient intubation during nCPAP reduces the need for MV without adverse effects on outcome and may be an option to more effectively treat RDS, particularly in a care setting where transfer is necessary to provide MV.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Berggren E, Liljedahl M, Winbladh B, Andreasson B, Curstedt T, Robertson B et al. Pilot study of nebulized surfactant therapy for neonatal respiratory distress syndrome. Acta Paediatr 2000; 89: 460–464.
Arroe M, Pedersen-Bjergaard L, Albertsen P, Bode S, Greisen G, Jonsbo F . Inhalation of aerosolized surfactant (Exosurf) to neonates treated with continuous positive airway pressure. Prenat Neonat Med 1998; 3: 346–352.
Dreyfuss D, Saumon G . Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med 1998; 157: 294–323.
Parker JC, Hernandez LA, Peevy KJ . Mechanisms of ventilator-induced lung injury. Crit Care Med 1993; 21: 131–143.
Bohlin K, Bouhafs RK, Jarstrand C, Curstedt T, Blennow M, Robertson B . Spontaneous breathing or mechanical ventilation alters lung compliance and tissue association of exogenous surfactant in preterm newborn rabbits. Pediatr Res 2005; 57: 624–630.
Van Marter LJ, Allred EN, Pagano M, Sanocka U, Parad R, Moore M et al. Do clinical markers of barotrauma and oxygen toxicity explain interhospital variation in rates of chronic lung disease? The Neonatology Committee for the Developmental Network. Pediatrics 2000; 105: 1194–1201.
Avery ME, Tooley WH, Keller JB, Hurd SS, Bryan MH, Cotton RB et al. Is chronic lung disease in low birth weight infants preventable? A survey of eight centers. Pediatrics 1987; 79: 26–30.
Victorin LH, Deverajan LV, Curstedt T, Robertson B . Surfactant replacement in spontaneously breathing babies with hyaline membrane disease – a pilot study. Biol Neonate 1990; 58: 121–126.
Verder H, Robertson B, Greisen G, Ebbesen F, Albertsen P, Lundstrom K et al. Surfactant therapy and nasal continuous positive airway pressure for newborns with respiratory distress syndrome. Danish-Swedish Multicenter Study Group. N Engl J Med 1994; 331: 1051–1055.
Verder H, Albertsen P, Ebbesen F, Greisen G, Robertson B, Bertelsen A et al. Nasal continuous positive airway pressure and early surfactant therapy for respiratory distress syndrome in newborns of less than 30 weeks' gestation. Pediatrics 1999; 103: E24.
Dani C, Bertini G, Pezzati M, Cecchi A, Caviglioli C, Rubaltelli F . Early extubation and nasal continuous positive airway pressure after surfactant treatment for respiratory distress syndrome among preterm infants <30 weeks gestation. Pediatrics 2004; 113: 560–563.
Reininger A, Khalak R, Kendig J, Ryan R, Stevens T, Reubens L et al. Surfactant administration by transient intubation in infants 29 to 35 weeks' gestation with respiratory distress syndrome decreases the likelihood of later mechanical ventilation: A randomized controlled trial. J Perinatol 2005; 25: 703–708.
Kamper J, Wulff K, Larsen C, Lindequist S . Early treatment with nasal continuous positive airway pressure in very low-birth-weight infants. Acta Paediatr 1993; 82: 193–197.
Jonsson B, Katz-Salamon M, Faxelius G, Broberger U, Lagercrantz H . Neonatal care of very-low-birthweight infants in special-care units and neonatal intensive-care units in Stockholm. Early nasal continuous positive airway pressure versus mechanical ventilation: gains and losses. Acta Paediatr Suppl 1997; 419: 4–10.
Hjalmarson O . Epidemiology and classification of acute, neonatal respiratory disorders. A prospective study. Acta Paediatr Scand 1981; 70: 773–783.
Benveniste D, Berg O, Pedersen JE . A technique for delivery of continuous positive airway pressure to the neonate. J Pediatr 1976; 88: 1015–1019.
Shennan A, Dunn M, Ohlsson A, Lennox K, Hoskins E . Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics 1988; 82: 527–532.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 1978; 92: 529–534.
Gobel W, Richard G . Retinopathy of prematurity – current diagnosis and management. Eur J Pediatr 1993; 152: 286–290.
Yost CC, Soll RF . Early versus delayed selective surfactant treatment for neonatal respiratory distress syndrome. Cochrane Database Syst Rev 2000; (2), CD001456.
Kamper J . Early nasal continuous positive airway pressure and minimal handling in the treatment of very-low-birth-weight infants. Biol Neonate 1999; 76 (Suppl 1): 22–28.
Verder H, Ebbesen F, Linderholm B, Robertson B, Eschen C, Arroe M et al. Prediction of respiratory distress syndrome by the microbubble stability test on gastric aspirates in newborns of less than 32 weeks' gestation. Acta Paediatr 2003; 92: 728–733.
Björklund LJ, Ingimarsson J, Curstedt T, John J, Robertson B, Werner O et al. Manual ventilation with a few large breaths at birth compromises the therapeutic effect of subsequent surfactant replacement in immature lambs. Pediatr Res 1997; 42: 348–355.
Jobe AH, Kramer BW, Moss TJ, Newnham JP, Ikegami M . Decreased indicators of lung injury with continuous positive expiratory pressure in preterm lambs. Pediatr Res 2002; 52: 387–392.
Speer CP, Robertson B, Curstedt T, Halliday HL, Compagnone D, Gefeller O et al. Randomized European multicenter trial of surfactant replacement therapy for severe neonatal respiratory distress syndrome: single versus multiple doses of Curosurf. Pediatrics 1992; 89: 13–20.
Stevens TP, Blennow M, Soll RF . Early surfactant administration with brief ventilation vs selective surfactant and continued mechanical ventilation for preterm infants with or at risk for respiratory distress syndrome. Cochrane Database Syst Rev 2004; (3), CD003063.
Acknowledgements
We thank the neonatal staff at Karolinska Huddinge and Solna for their support and skilled care of these infants. This work was supported by grants from the Swedish Society of Medicine and the Swedish Freemasons in Stockholm Foundation for Children's Welfare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bohlin, K., Gudmundsdottir, T., Katz-Salamon, M. et al. Implementation of surfactant treatment during continuous positive airway pressure. J Perinatol 27, 422–427 (2007). https://doi.org/10.1038/sj.jp.7211754
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211754
Keywords
This article is cited by
-
A clinical study evaluating the combination of LISA and SNIPPV for the treatment of respiratory distress syndrome in preterm infants
Scientific Reports (2024)
-
Retrospective comparison of death or neurodevelopmental outcomes in extremely low birth weight preterm infants following different management options of haemodynamically significant patent ductus arteriosus
BMC Pediatrics (2021)
-
A novel delivery system for supraglottic atomization allows increased lung deposition rates of pulmonary surfactant in newborn piglets
Pediatric Research (2020)
-
Surfactant replacement therapy: from biological basis to current clinical practice
Pediatric Research (2020)
-
Effectiveness of intratracheal salbutamol in addition to surfactant on the clinical course of newborns with respiratory distress syndrome: a clinical trial
Italian Journal of Pediatrics (2016)