Abstract
Objective:
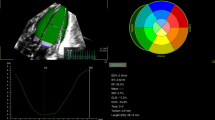
To determine the accuracy of the patent ductus arteriosus:left pulmonary artery ratio (PDA:LPA) on echocardiogram (ECHO) at 3-day postnatal in predicting spontaneous PDA closure in neonates ⩽30 weeks gestational age (GA).
Study Design:
ECHOs were performed at 72 h to characterize PDA size as closed-to-small (PDA:LPA <0.5) or moderate-to-large (PDA:LPA ⩾0.5) and at 10 days to determine spontaneous closure (defined as closed-to-small in the absence of medical and/or surgical treatment). Caretakers were blinded to results; treatment was based on standard care. Neonates were prospectively enrolled and stratified: <27 weeks (n=31) and 27 to 30 weeks (n=65).
Result:
Neonates <27 weeks with closed-to-small PDAs had 60% spontaneous closure vs 9% when moderate-to-large (positive predictive value (PPV) 60%, negative predictive value (NPV) 91%). Neonates 27 to 30 weeks had 95% spontaneous closure vs 27%, respectively (PPV 95%, NPV 73%). Inter-observer variability for the initial ECHO was 0.84.
Conclusion:
PDA size defined by PDA:LPA at 3 days postnatal in combination with GA predicts spontaneous PDA closure.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Shimada S, Kasai T, Konishi M, Fujiwara T . Effects of patent ductus arteriosus on left ventricular output and organ blood flows in preterm infants with respiratory distress syndrome treated with surfactant. J Pediatr 1994; 125: 270–277.
Bancalari E . Changes in the pathogenesis and prevention of chronic lung disease of prematurity. Am J Perinatol 2001; 18: 1–9.
Jim WT, Chiu NC, Chen MR, Hung HY, Kao HA, Hsu CH et al. Cerebral hemodynamic change and intraventricular hemorrhage in very low birth weight infants with patent ductus arteriosus. Ultrasound Med Biol 2005; 31: 197–202.
Cassady G, Crouse DT, Kirklin JW, Strange MJ, Joiner CH, Godoy G et al. A randomized, controlled trial of very early prophylactic ligation of the ductus arteriosus in babies who weighted 1000 gm or less at birth. N Engl J Med 1989; 320: 1511–1516.
Kabra NS, Schmidt B, Roberts RS, Doyle LW, Papile L, Fanaroff A . Neurosensory impairment after surgical closure of patent ductus arteriosus in extremely low birth weight infants: results from the Trial of Indomethacin Prophylaxis in Preterms. J Pediatr 2007; 150: 229–234.
Clyman RI . Recommendations for the postnatal use of indomethacin: an analysis of four separate treatment strategies. J Pediatr 1996; 128: 601–607.
Bose CL, Laughon MM . Patent ductus arteriosus: lack of evidence for common treatments. Arch Dis Child Fetal Neonatal Ed 2007; 92: F498–F502.
Benitz WE . Treatment of persistent patent ductus arteriosus in preterm infants: time to accept the null hypothesis? J Perinat 2010; 30: 241–252.
Hamrick SE, Hansmann G . Patent ductus arteriosus of the preterm infant. Pediatrics 2010; 125: 1020–1030.
Fowlie PW, Davis PG . Prophylactic indomethacin for preterm infants: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 2003; 88: F464–F466.
Jones LJ, Craven PD, Attia J, Thakkinstian A, Wright I . Network meta-analysis of indomethacin versus ibuprofen versus placebo for PDA in preterm infants. Arch Dis Child Fetal Neonatal Ed 2011; 96: F45–F52.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 2010; 126: 443–456.
Gonzalez VI, Ferrer NC, Pueyo RV, Garcia ME, Rite GS, Caballero PV et al. [Is patent ductus arteriosus a risk factor for retinopathy of prematurity?]. An Pediatr (Barc) 2011; 74: 25–30.
Van Overmeire B, Van de Broek H, Van Laer P, Weyler J, Vanhaesebouck P . Early versus late indomethacin treatment for patent ductus arteriosus in premature infants with respiratory distress syndrome. J Pediatr 2001; 138: 205–211.
Koch J, Hensley G, Roy L, Brown S, Ramaciotti C, Rosenfeld CR . Prevalence of spontaneous closure of the ductus arteriosus in neonates at a birth weight of 1000 grams or less. Pediatrics 2006; 117: 1113–1121.
Narayanan M, Cooper B, Weiss H, Clyman RI . Prophylactic indomethacin: factors determining permanent ductus closure. J Pediatr 2000; 136: 330–337.
Ramos FG, Rosenfeld CR, Roy L, Koch J, Ramaciotti C . Echocardiographic predictors of symptomatic patent ductus arteriosus in extremely-low-birth-weight preterm neonates. J Perinatol 2010; 30: 535–539.
Wald RM, Adatia I, Van Arsdell GS, Hornberger LK . Relation of limiting ductal patency to survival in neonatal Ebstein's anomaly. Am J Cardiol 2005; 96: 851–856.
Skelton R, Evans N, Smythe J . A blinded comparison of clinical and echocardiographic evaluation of the preterm infant for patent ductus arteriosus. J Paediatr Child Health 1995; 30: 406–411.
Chirovulu A, Jaleel MA . Therapeutic management of patent ductus arteriosus. Early Hum Dev 2009; 85: 151–155.
Sehgal A, McNamara PJ . Does echocardiography facilitate determination of hemodynamic significant attributable to the ductus arteriosus? Eur J Pediatr 2009; 168: 907–914.
Silverman NH, Lewis AB, Heymann MA, Rudolph AM . Echocardiographic assessment of ductus arteriosus shunt in premature infants. Circulation 1974; 50: 821–825.
Kluckow M, Evans N . Early echocardiographic prediction of symptomatic patent ductus arteriosus in preterm infants undergoing mechanical ventilation. J Pediatr 1995; 127: 774–779.
Shah SS, Ohlsson A . Ibuprofen for the prevention of patent ductus arteriosus in preterm and/or low birth weight infants. Cochrane Database Syst Rev 2006; CD004213.
Nemerofsky SL, Parravicini E, Bateman D, Kleinman C, Polin RA, Lorenz JM . The ductus arteriosus rarely requires treatment in infants >1000 grams. Am J Perinatol 2008; 25: 661–666.
Harling S, Hansen-Pupp I, Baigi A, Pesonen E . Echocardiographic prediction of patent ductus arteriosus in need of therapeutic intervention. Acta Pediatr 2011; 100: 231–235.
Iyer P, Evans N . Re-evaluation of the left atrial to aortic root ratio as a marker of patent ductus arteriosus. Arch Dis Child Fetal Neonatal Ed 1994; 70: F112–F117.
Hirschklau MJ, DiSessa TG, Higgins CB, Friedman WF . Echocardiographic diagnosis: pitfalls in the premature infant with a large patent ductus arteriosus. J Pediatr 1978; 92: 474–477.
Simpson IA, Sahn DJ, Valdes-Cruz LM, Chung KJ, Sherman FS, Swensson RE . Color Doppler flow mapping in patients with coarctation of the aorta: new observations and improved evaluation with color flow diameter and proximal acceleration as predictors of severity. Circulation 1988; 77: 736–744.
Ramaciotti C, Lemler MS, Moake L, Zellers TM . Comprehensive assessment of patent ductus arteriosus by echocardiography before transcatheter closure. J Am Soc Echocardiogr 2002; 15: 1154–1159.
Benitz WE . Patent ductus arteriosus: to treat or not to treat? Arch Dis Child Fetal Neonatal 2012; 97: F80–F82.
Noori S . Patent ductus arteriosus in the preterm infant: to treat or not to treat? J Perinat 2010; 30: S31–S37.
Clyman RI, Chorne N . Patent ductus arteriosus: evidence for and against treatment. J Pediatr 2007; 150: 216–219.
Acknowledgements
We thank Rong Huang, PhD, who helped with the biostatistical analysis of this study. Dr Rosenfeld is the recipient of the George L MacGregor Professorship in Pediatrics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Thankavel, P., Rosenfeld, C., Christie, L. et al. Early echocardiographic prediction of ductal closure in neonates ⩽30 weeks gestation. J Perinatol 33, 45–51 (2013). https://doi.org/10.1038/jp.2012.41
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2012.41
Keywords
This article is cited by
-
Defining information needs in neonatal resuscitation with work domain analysis
Journal of Clinical Monitoring and Computing (2021)
-
Early prediction of spontaneous Patent Ductus Arteriosus (PDA) closure and PDA-associated outcomes: a prospective cohort investigation
BMC Pediatrics (2019)
-
Exploration of potential biochemical markers for persistence of patent ductus arteriosus in preterm infants at 22–27 weeks’ gestation
Pediatric Research (2019)
-
Application of Neonatologist Performed Echocardiography in the assessment of a patent ductus arteriosus
Pediatric Research (2018)
-
Intravenous paracetamol for PDA closure in the preterm: a single-center experience
European Journal of Pediatrics (2016)