Abstract
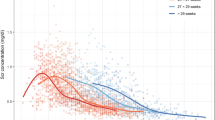
To document trends and covariates of creatinemia (Scr) in extremely low birth weight (ELBW, < 1,000 g) neonates, maternal characteristics [betamethasone, premature preterm rupture of membranes (PPROM), pre-eclampsia, maternal Scr], characteristics at delivery [gestational age (GA), birth weight (BW), small for GA (SGA), Apgar, intubation] and during neonatal stay [ventilation, oxygen, parenteral nutrition, ibuprofen, steroids, intraventricular hemorrhage, retinopathy of prematurity (ROP), phototherapy] were linked with Scr observations. Data were reported by median and range or incidence. Characteristics in ELBW neonates with raised peak Scr (>P75) were compared to controls (<P75). In 151 ELBW neonates, an initial increase in Scr was observed, resulting in a peak Scr on day 3 or 4 of 99.9 (46.8–221.8) μmol/l with subsequent decrease. In cases (n = 37) with a peak Scr >P75 (112.3 μmol/l), Scr remained elevated until day 28. Mothers of cases received less betamethasone, neonates had a lower GA, lower BW, lower Apgar, and needed more often intubation. Postnatal ventilation, oxygen, parenteral nutrition, ibuprofen, steroids, ROP, and intraventricular hemorrhage were different. GA and ventilation or Apgar were independent factors for raised peak Scr. ELBW neonates display trends similar to heavier neonates, but peak Scr is higher, and the subsequent decrease slower. Raised creatinemia in ELBW neonates reflects immaturity (GA) and morbidity (ventilation, Apgar).




Similar content being viewed by others
References
Cataldi L, Leone R, Moretti U, De Mitri B, Fanos V, Ruggeri L, Sabatino G, Torcasio F, Zanardo V, Attardo G, Riccobene F, Martano C, Benini D, Cuzzolin L (2005) Potential risk factors for development of acute renal failure in preterm newborn infants: a case control study. Arch Dis Child Fetal Neonatal Ed 90:F514–F519
Cuzzolin L, Fanos V, Pinna B, de Marzio M, Perin M, Tramontozzi P, Tonetto P, Cataldi L (2006) Postnatal renal function in preterm newborns: a role of diseases, drugs and therapeutic interventions. Pediatr Nephrol 21:931–938
Drukker A, Guignard JP (2002) Renal aspects of the term and preterm infant: a selective update. Curr Opin Pediatr 14:175–182
Bueva A, Guignard JP (1994) Renal function in preterm neonates. Pediatr Res 36:572–577
Van den Anker JN, Allegaert K (2009) Individualized dosing of aminoglycosides in neonates: mission accomplished or work in progress? Eur J Clin Pharmacol 65:1159–1160
Keijzer-Veen MG, Dülger A, Dekker FW, Nauta J, van der Heijden BJ (2010) Very preterm birth is a risk factor for increased systolic blood pressure at a young adult age. Pediatr Nephrol 25:509–516
Keijzer-Veen M, Devos AS, Meradji M, Dekker FW, Nauta J, van der Heijden BJ (2010) Reduced renal length and volume 20 years after very preterm birth. Pediatr Nephrol 25:499–507
Bachetta J, Harambat J, Dubourg L, Guy B, Liutkus A, Canterino I, Kassai B, Putet G, Cochat P (2009) Both extrauterine and intrauterine growth restriction impair renal function in children born very preterm. Kidney Int 76:445–452
Zaffanello M, Brugnara M, Bruno C, Franchi B, Talamini G, Guidi G, Cataldi L, Biban P, Mella R, Fanos V (2010) Renal function and volume of infants born with a very low birth-weight: a preliminary cross-sectional study. Acta Paediatr 99:1192–1198
Puddu M, Fanos V, Podda F, Zaffanello M (2009) The kidney for prenatal to adult life: perinatal programming and reduction of number of nephrons during development. Am J Nephrol 30:162–170
Vieux R, Hascoet JM, Merdariu D, Fresson J, Guillemin F (2010) Glomerular filtration rate reference values in very preterm children. Pediatrics 125:e1186–e1192
Guignard JP, Drukker A (1999) Why do newborn infants have a high plasma creatinine? Pediatrics 103:e49
Allegaert K, Anderson BJ, van den Anker JN, Vanhaesebrouck S, de Zegher F (2007) Renal drug clearance in preterm neonates: relation to prenatal growth. Ther Drug Monit 29:284–291
Boer DP, de Rijke YB, Hop WC, Cransberg K, Dorresteijn EM (2010) Reference values for serum creatinine in children younger than 1 year of age. Pediatr Nephrol 25:2107–2113
Rudd PT, Hughes EA, Placzek MM, Hodes DT (1983) Reference ranges for plasma creatinine during the first month of life (1983). Arch Dis Child 58:212–215
Gallini F, Maggio L, Romagnoli C, Marrocco G, Tortorolo G (2000) Progression of renal function in preterm neonates with gestational age ≤ 32 weeks. Pediatr Nephrol 15:119–124
Thayyil S, Sheik S, Kempley ST, Sinha A (2008) A gestation- and postnatal age-based reference chart for assessing renal function in extremely premature infants. J Perinatol 28:226–229
Iacobelli S, Bonsante F, Ferdinus C, Labenne M, Gouyon JB (2009) Factors affecting postnatal changes in serum creatinine in preterm infants with gestational age <32 weeks. J Perinatol 29:232–236
Vieux R, Desandes R, Boubred F, Semama D, Guillemin F, Buchweiller MC, Fesson J, Hascoet JM (2010) Ibuprofen in very preterm infants impairs renal function for the first month of life. Pediatr Nephrol 25:267–274
Allegaert K, Cossey V, Debeer A, Langhendries JP, Van Overmeire B, de Hoon J, Devlieger H (2005) The impact of ibuprofen on renal clearance in preterm infants in independent of the gestational age. Pediatr Nephrol 20:740–743
Abitbol CL, Bauer CR, Montané B, Chandar J, Duara S, Zilleruelo G (2003) Long-term follow-up of extremely low birth weight infants with neonatal renal failure. Pediatr Nephrol 18:887–893
Acknowledgements
Elena Levtchenko and Karel Allegaert are supported by the Fund for Scientific Research, Flanders (Belgium) (F.W.O. Vlaanderen) by a Fundamental Clinical Investigatorship (1801110 N and 1800209 N).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
George, I., Mekahli, D., Rayyan, M. et al. Postnatal trends in creatinemia and its covariates in extremely low birth weight (ELBW) neonates. Pediatr Nephrol 26, 1843–1849 (2011). https://doi.org/10.1007/s00467-011-1883-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-011-1883-0