Abstract
Aims To ascertain how closely services for the screening and treatment of retinopathy of prematurity (ROP) were organised on a national level in 1995.
Methods Questionnaires about the local arrangements for the screening and treatment of retinopathy of prematurity (ROP) were sent to the entire consultant membership (n = 648) of the Royal College of Ophthalmologists (RCOphth) and to the clinical directors (n = 259) of neonatal units and other units caring for preterm babies in the UK in 1995.
Results 568/648 of UK consultants (88%) and 15 non-consultant ophthalmologists and 210/259 paediatricians (81%) and 19% paediatricians in non-neonatal units responded. Thirty-one per cent responding ophthalmologists were involved in the ROP service: of these 64% screened babies, 34% screened and treated babies, while 1% ophthalmologists treated ROP but did not screen. Ninety-six per cent units caring for preterm babies had their babies screened for ROP and for almost 95% of the screening took place in the neonatal unit. About 8200 babies were screened in 1994; 277 developed stage 3, of whom 54% received treatment. Nine per cent (n = 14) and 5% (n = 8) treated babies became blind in one and both eyes respectively. A sessional commitment was identified for 9% ophthalmologists, but for less than half this was included in the contracted work programme. Sixty-five ophthalmologists treated babies with ROP, but only 10 treated more than five babies in 1994. Training needs were identified by 71 respondents.
Conclusions Several aspects of ROP screening and treatment services require improvement. Hopefully, reducing the number of identified screeners would increase skills, confidence and the ability to recognise severe disease requiring treatment, and also facilitate incorporation of this work into consultant work plans.
Similar content being viewed by others
Introduction
Retinopathy of prematurity (ROP) is a potentially blinding condition affecting babies born prematurely. First described as retrolental fibroplasia in the 1940s, it was about two decades later that treatment was first attempted, although results were inconclusive due to a number of factors which included the absence of an adequate disease classification. With no effective preventative or therapeutic measures, screening was not considered a priority in the UK, until the publication of an international classification for ROP in 1984.1 This permitted, for the first time, comparison between centres and generated a wave of clinical research. Foremost of these was the Multicenter Trial of Cryotherapy for ROP (CRYO-ROP Study) which in 1988 demonstrated for the first time the efficacy of treatment for severe disease.2 Screening then became a priority, and in response, the British Association of Perinatal Medicine and the Royal College of Ophthalmologists in 1990 drew up guidelines3 which were revised in 1995.4
ROP is described by stages numbered 1–5. Disease not progressing beyond stages 1 and 2 is referred to as mild because these stages resolve without adverse effects on vision. Stages 3–5 are severe as they have the potential for causing vision impairment. At stages 4 and 5, retinal detachment is present and treatment is not effective. Screening, is therefore directed to identify stage 3 ROP, as a subdivision of this stage—‘threshold’ ROP is the current indication for treatment by laser surgery or cryotherapy. ‘Threshold’, is the stage at which, it is the consensus opinion that the risk of blindness, if untreated, is about 50% and is defined as stage 3 ROP in zone 1 or 2, extending over five or more contiguous, or eight or more cumulative, clock hours of the retinal circumference, in the presence of ‘plus’ disease.2 Plus disease is an indicator of ROP activity and in order of increasing severity, the signs include: engorgement and tortuosity of the posterior pole retinal vessels, iris vessel engorgement, pupil rigidity and vitreous haze.
The increasing survival of very low birthweight babies presents a particular challenge to those professionals responsible for ensuring that all babies at risk of ROP are screened. Most low birthweight premature babies develop some degree of ROP although more severe disease is relatively infrequent.5,6 In the CRYO-ROP Study, 66% of 4099 babies <1251 g birthweight developed some ROP, which later progressed to stage 3 in 18%, reaching threshold in 6%.2 A comprehensive screening and treatment programme has therefore to screen a relatively large population of babies at risk in order to identify those few who might develop severe disease. Furthermore rapid rate of progression for severe disease6 means that once detected treatment has to be given within a very short space of time. This ‘short space of time’ is empirically derived to minimise the risk of progression to a stage when treatment effectivity is reduced, and in the CRYO-ROP Study was limited to 72 hours.2
ROP screening and its subsequent management require the involvement of staff in neonatal units and the ophthalmologists who undertake the eye examinations. This multiprofessional involvement requires a high degree of co-operation as well as clear agreement about which babies are at risk and, when and how often screening should take place. Ensuring that every baby at risk is screened appropriately can be complicated by the fact that some are clinically unstable while others are discharged home or transferred to another hospital before screening is complete. These practical considerations place further demands on the joint working arrangements of the ophthalmologists and the neonatal team, leading to concern that some babies may be slipping through the net and not being screened appropriately.
In 1995 a 5-year programme of research was begun by the Royal College of Paediatrics and Child Health (then the British Paediatric Association), the Royal College of Ophthalmologists and the British Association for Perinatal Medicine to improve the identification and treatment of ROP in the UK. The first phase of the research was a survey of the services for ROP screening and treatment in the UK to examine how services were organised and to audit adherence to recommendations in national guidelines. This paper reports the findings in relation to service organisation in 1995. The detailed findings of the audit of national guidelines are presented in the accompanying paper.
Methodology
Questionnaires about the local arrangements for the screening and treatment of ROP were sent to the entire consultant membership (648) of the Royal College of Ophthalmologists (RCOphth) and to the clinical directors (259) of all the neonatal units in the UK. Circulation was later extended on the basis of information supplied on the neonatal unit questionnaire to include non-consultant ophthalmologists who were screening for ROP and non-neonatal units receiving transfers of babies at risk of ROP (ie paediatric surgical or intensive care units). Non-responders were followed up with a second mailing and two telephone reminders.
Results
Eighty-eight per cent (568/648) of consultant ophthalmologists and 15 non-consultants responded giving a total of 583 questionnaires from ophthalmologists. Eighty-one per cent (210/259) of paediatricians and 19% (6/32) of paediatricians in non-neonatal units completed questionnaires.
Of the ophthalmologists surveyed, 31% (183/583) were involved in the ROP service; 64% (118) screened babies, 34% (63) screened and treated babies and 1% (2) ophthalmologists treated ROP but did not screen. Detailed information was provided by 182 individuals.
There were 216 replies from clinicians in units caring for premature babies; 210 were neonatal units, three were paediatric intensive care units, two were neonatal surgical units and one a children’s surgical ward. Overall, 96% (207) screened babies for ROP: 205 in neonatal units and two in non-neonatal units (some very infrequently cared for premature babies). Thus, there was screening in 98% of the neonatal units responding to the survey (205/210).
Of the nine units not screening for ROP, five were neonatal units. Staff in four commented on the lack of screening; two cited a shortage of appropriately trained ophthalmologists, one transferred eligible babies to another hospital and the fourth acknowledged that ROP screening needed urgent consideration. Of the four non-neonatal units in which there was no screening, one was a general PICU and three were neonatal surgical units.
Service delivery—location
Most ROP screening took place within the neonatal unit; in 95% (197) of units all eligible babies were screened on the unit, 36 units transferred some babies to another hospital for screening and four units transferred all their babies who required screening. Six units transferred babies within the hospital. Ophthalmologists confirmed these practices; 80% of the locations where ophthalmologists screened were neonatal units and 20% were outpatient departments; one ophthalmologist also screened in a cardiac intensive care unit.
Screening frequency
The clinical directors of neonatal units were asked how many babies were screened from 1992–1994 and ophthalmologists were asked about their personal screening practice in a single year, 1994.
Data provided by the ophthalmologists were the most complete; 89% (152/170) of the ophthalmologists in the same post in 1994 gave numbers although these were often approximate or a range. In comparison only 67% of units (139) could provide data for 1994, while for 1992 and 1993 data collection was even poorer. In total (taking the upper figure of a range), the 152 ophthalmologists screened 8208 babies in 1994, compared with 5985 babies screened in the neonatal units providing data. The fact that only two thirds of units could provide numbers of babies screened could be explained by the finding that only 54% of the units (112/207) had a specific book for recording babies’ screening status.
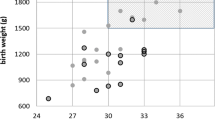
ROP screening is an infrequent activity in neonatal units; of the 139 units providing data, 71% (100/139) screened fewer than 50 babies, 24% screened 50–100 and only 4% (6) units screened over 100 babies in 1994. Similarly ROP screening is an infrequent activity for many ophthalmologists; the number of babies screened in 1994 by the 152 ophthalmologists providing data is illustrated in Figure 1; 55% (83) screened 40 or fewer babies, 18% (27) screened 41–70 babies, and only just under a quarter (24%, (37)) screened over 70 babies.
Two thirds of ophthalmologists (66%, 98/148) spent less than half a session a week ROP screening; 26% (n = 38) spent half to one session, and only 8% (n = 12) screened for at least one session. Screening was also unlikely to be identified in a consultants work programme and this was the case for over half of the ophthalmologists (58%, 104/180). For 27% (48/180), ROP screening was identified in the work programme but had no specific sessional commitment and only 9% (17/180) had a sessional commitment identified. Sixteen of the 37 ophthalmologists who screened more than 70 babies in 1994 did not have ROP screening identified in their work plan, including one who spent three sessions a week screening babies.
Services for ROP treatment
Sixty-five ophthalmologists surveyed undertook ROP treatment. Of these 62 were consultants, two were non-consultant non-trainees and one a senior registrar. In 1995, 80% (52/65) of ophthalmologists used cryotherapy although 59% also used laser.
Sixty-one ophthalmologists identified a total of 76 different locations where they treated babies: 62% neonatal units (47/76); 37% operating theatres (28/76) and one was an outpatient department. Most ophthalmologists (80%, 49/61) only treated babies in a single hospital although 10 treated in two hospitals and two in three hospitals.
The paediatricians’ replies suggested that ROP treatment was more centralised than screening. Over half of the units, 55% (93/168) transferred babies to another hospital, 31% (52) treated babies on the unit, and 14% (23) transferred babies to the hospital’s ophthalmology department.
Ophthalmologists treating babies for ROP were asked how many babies with stage 3 ROP they had assessed for treatment, the number treated, and the number treated who developed end-stage blinding ROP in one or both eyes in 1992–1994. The results which are shown in Table 1 confirm that severe ROP requiring treatment is infrequent. In 1994, 277 babies with stage 3 ROP were assessed for treatment. Of the 65 ophthalmologists who treated ROP only just over half (57%, 37/65) treated any babies in 1994 and the greatest number treated by a single ophthalmologist was 17 with only three treating more than 10 babies. Six individuals treated 5–10 babies and 29 treated fewer than 5.
According to survey data, between 1992–1994 the number of treated babies who became blind in one or both eyes was 22, 20 and 23 respectively. The survey however undoubtedly underestimates the visual morbidity caused by ROP, as babies untreated and those with lesser, but functionally significant vision impairment, were not included in the figures.
Ophthalmologists and neonatal clinical directors were asked to comment on the organisation of ROP services, identifying potential improvements or training needs. Fifty-three per cent (n = 10) of the clinical directors commented, highlighting good and bad aspects of current practice. Poor recording of data on ROP screening on the unit was noted several times, as was the need to provide information for parents. Other improvements recommended were an increased awareness of the need to refer babies at risk to the ophthalmologists, as well as improved communication between the unit and ophthalmologists and between units if babies are transferred.
In all, 92 ophthalmologists commented on the organisation of services in their locality; several (n=11) felt that services were haphazard or ad hoc. Other problems identified were a lack of interest by paediatricians, no dedicated sessions for screening, no funding for sessions, no agreement about who pays for equipment, and the difficulty of arranging cover for annual leave and study leave.
Comments on training needs were made by 71 ophthalmologists. Although quantitative analysis of this information was not possible, it is clear from the number who commented that training for ROP screening and treatment needs to be addressed, initially to include ROP screening into training programmes for trainees, followed by ongoing training for consultants. Some commented that the rarity of severe ROP meant that even those regularly screening needed continuing education. Suggestions for how this might be delivered included visits to specialist units taking referrals for ROP management, organised study days or practical sessions, videos and slides, more consultant time for training, dissemination of regular updates and guidelines, wall charts and protocols for neonatal units as well as specific training on treatment techniques.
Discussion
The survey reported here is the first national survey of ROP screening and treatment. It provides an overview of the organisation of services in the UK in 1995 from the perspective of ophthalmologists and paediatricians involved in the service. The response to the survey was good with 81% of clinical directors of neonatal units and 88% of ophthalmologists returning questionnaires.
The survey showed that by 1995, 5 years after the first national guidelines, screening programmes for ROP had been established in most neonatal units across the UK with screening in 96% responding units and 79% of all UK neonatal units (205/259) and 71% (207/291) of all UK units that cared for premature babies. The last figure includes units that may care only infrequently for premature babies, although it should be noted that these units may receive babies for surgery (for instance), at a time when severe ROP is most likely to occur. These ROP services were being delivered by at least 183 ophthalmologists, most screening babies in the neonatal unit of a single hospital. The organisation of ROP screening services consisted of a small number of ‘super-screeners’ screening large numbers of babies (37 individuals screened 60% of all babies screened in 1994) and a larger number for whom ROP screening was an infrequent activity.
Because ophthalmologists screen small numbers of babies and with a low incidence of severe ROP, it is possible that these individuals do not screen enough to reliably recognise severe disease. Furthermore for most ophthalmologists the workload associated with ROP screening had not in 1995 been recognised contractually or identified in consultants’ work plan. It is of concern that even the ophthalmologists screening large numbers of babies appeared not to have a specific sessional commitment allocated for this work.
In contrast to ROP screening, the services for treatment in the UK were more concentrated. Only 65 ophthalmologists treated babies in 1995, although at least a third had not treated any babies the year before. As with the screening, workload was not evenly distributed and only 10 individuals treated more than five babies. In 1995 cryotherapy was the treatment of choice although already there was an emerging trend towards the use of laser therapy which has continued to the present.
The incidence of severe ROP reported by ophthalmologists in the survey was in line with data from previous studies in spite of the fact that the figures were approximate and could include duplicate cases. In 1994 277 babies with stage 3 ROP were assessed for treatment, approximately 3.4% of the estimated screened population of 8206. The treatment rates ascertained from study data were also broadly similar to both CRYO-ROP and LIGHT-ROP Studies which were separated by a decade.7,8 Direct comparison is not possible because both of these studies included only babies of less than 1250 grams birthweight. In all 1.8% of screened babies in the UK required treatment, around 54% of all babies with stage 3 assessed for treatment.
It is well documented2,6 that even with optimal screening and treatment some babies still suffer from visual morbidity due to ROP. Between 9% and 12% of babies treated between 1992 and 1994 became blind in one eye and approximately 5% each year became blind bilaterally. These figures however cannot be used to estimate treatment success as, for some babies, it may have been recognised at the time that treatment was too late to rescue any functional sight. The figures are also an underestimate of the total number of babies in the UK suffering ROP-induced severe visual morbidity due to underreporting and exclusion of babies not receiving any treatment.
The survey identified several aspects of ROP screening and treatment services that require attention. Organising the screening services so that districts have a small number of identified screeners who undertake screening more regularly would increase skills and confidence and the ability to recognise severe disease requiring treatment. With fewer ophthalmologists screening more babies there could be no argument for not identifying this activity in consultants work plans and making a sessional commitment for this work. That would include travel time and sufficient time to communicate the results and likely prognosis to parents.
The questionnaires highlighted that in 1995 there were substantial training needs for both junior staff and consultants. Screening premature babies for ROP and recognising rapidly progressing disease is a highly specialised activity which requires specialised training although the rarity of severe ROP means that it is seen infrequently even by regular screeners. A regular audit of screening practice against nationally agreed guidelines should be undertaken and consultants should have the opportunity for clinical updates. Although it is suggested that services are reorganised so that fewer ophthalmologists undertake screening, the inclusion of ROP screening in the specialist training for ophthalmologists is important. The Northern Region of England has regionalised ROP services with the effect of increasing guideline compliance.9
With less than 2% of screened babies requiring treatment, there is also an argument for concentrating ROP treatment services still further so that ophthalmologists treating babies undertake the procedure more frequently to maintain skills.
Although there is, as yet, no clinical evidence that treatment outcome is related to the level of experience of the treating ophthalmologist, restricting ROP treatment to tertiary centres would concentrate resources and expertise and would facilitate further research into outcomes of treatment. However regardless of how treatment services are organised geographically, it is essential that they are staffed to facilitate cross cover for sickness and annual leave, because of the short window of opportunity for the effective treatment of severe ROP. As mentioned in the introduction, this paper is the result of the first phase of a 5-year programme of research to improve the identification and treatment of ROP in the UK. The results presented herein therefore form the basis for the second phase, a prospective 15-month study of stage 3 ROP, its diagnosis and management which commenced in 1997. Following analysis of the second phase of research, audit guidelines and recommendations for future practice will be produced.
References
Committee for the Classification of Retinopathy of Prematurity. An international classification of retinopathy of prematurity. Br J Ophthalmol 1984; 68: 690–697
Cryotherapy for Retinopathy of Prematurity Cooperative Group. Multicenter trial of cryotherapy for retinopathy of prematurity: preliminary results. Arch Ophthalmol 1988; 106: 471–479
Anon . College News: ROP screening duty. Quart Bull Coll Ophthalmol 1990; (autumn): 6
Report of a Joint Working Party. The Royal College of Ophthalmologists, British Association of Perinatal Medicine. Retinopathy of prematurity: guidelines for screening and treatment. Early Human Dev 1996; 46: 239–258
Fielder A R, Levene M I . Screening for retinopathy of prematurity. Arch Dis Child 1992; 67: 860–867
Clemett R, Darlow B . Results of screening low-birth-weight infants for retinopathy of prematurity. Curr Opin Ophthalmol 1999; 10: 155–163
Palmer EA, Flynn JT, Hardy RJ, Phelps DL, Phillips CL, Schaffer DB et al. The Cryotherapy for Retinopathy of Prematurity Cooperative Group. Incidence and early course of retinopathy of prematurity. Ophthalmology 1991; 98: 1628–1640
Reynolds JD, Hardy RJ, Kennedy KA, Spencer R, van Heuven WAJ, Fielder AR for the Light Reduction in Retinopathy of Prematurity (LIGHT-ROP) Cooperative Group. Lack of efficacy of light reduction in preventing retinopathy of prematurity. New Eng J Med 1998; 338: 1572–1576
Ziakas NG, Cottrell DG, Milligan DWA, Pennefather PM, Bamashmus MA, Clarke MP . Regionalisation of retinopathy of prematurity (ROP) screening improves compliance with guidelines: an audit of ROP screening in the Northern Region of England. Br J Ophthalmol 2001; 85: 807–810
Acknowledgements
This study was funded by the Department of Health. We are very grateful to the Royal Colleges of Ophthalmologists and Paediatrics and Child Health for facilitating and supporting this study, and to all the ophthalmologists and clinical directors of UK neonatal units who took the time to complete the study questionnaires.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Haines, L., Fielder, A., Scrivener, R. et al. Retinopathy of prematurity in the UK I: The organisation of services for screening and treatment. Eye 16, 33–38 (2002). https://doi.org/10.1038/sj.eye.6700030
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700030
Keywords
This article is cited by
-
Validation of WINROP (online prediction model) to identify severe retinopathy of prematurity (ROP) in an Australian preterm population: a retrospective study
Eye (2021)
-
Children’s Hospital of Philadelphia Score to predict severe retinopathy in Indian preterm infants
Eye (2019)
-
Preterm-associated visual impairment and estimates of retinopathy of prematurity at regional and global levels for 2010
Pediatric Research (2013)
-
Variation in anaesthesia for the laser treatment of retinopathy of prematurity—a survey of ophthalmologists in the UK
Eye (2007)
-
Time for a fresh look at ROP screening
Eye (2003)